Research Article - (2025) Volume 20, Issue 6
Assess Artificial Intelligence In Emergency Medicine For Better Patient Care A Systematic Review
Atef Eid Madkour Elsayeda1*, Mohsin Shahabuddin1, Abdulrahman Emad Shafie2, Fadi Elshafi Babikir Mohammed3*, Abid Waseem4, Muneer Ahmed Mohammed Bakr5, Waheed Ibrahim Mohamed Alasiri6, Ghaliah Waleed Hamid Othman7, Sayyaf Mohammed Alhazmi8 and Imtiaz Ahmed S/0 Muhammad Soomar Soomro9*Correspondence: Atef Eid Madkour Elsayeda, Consultant, King Abdelaziz Hospital, Sakaka, Saudi Arabia, Email: Fadi Elshafi Babikir Mohammed, Emergency medicine physician, Saudi Arabia,
2Medicine and surgery, Saudi Arabia
3Emergency medicine physician, Saudi Arabia
4Emergency medicine physician, Saudi Arabia
5Emergency medicine, Saudi Arabia
6General practitioner, Saudi Arabia
7General Practitioner, Saudi Arabia
8General practitioner, Saudi Arabia
9Emergency physician, Saudi Arabia
Received: 10-Oct-2025 Published: 24-Nov-2025
Abstract
Background: Artificial intelligence (AI) has emerged as a transformative tool in emergency medicine, where timely and accurate decision-making is vital. Machine learning (ML), deep learning (DL), and natural language processing (NLP) approaches are increasingly applied to enhance triage, risk stratification, and prediction of adverse outcomes. Despite these advances, variability in methodologies and reported outcomes underscores the need for a systematic synthesis of the evidence.
Objective: This systematic review evaluates the impact of AI in emergency medicine, focusing on its influence on triage accuracy, clinical outcomes, workflow efficiency, and overall patient care.
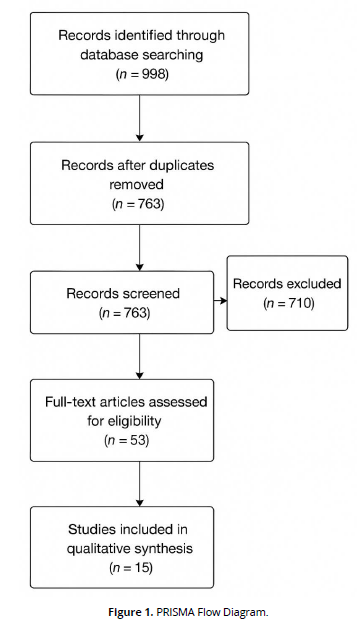
Methods: The review was conducted in line with PRISMA 2020 guidelines. Eligible studies included randomized controlled trials, retrospective and prospective cohorts, and case-control designs assessing AI use in emergency or critical care. Literature searches were performed across PubMed, Scopus, Web of Science, Embase, and IEEE Xplore (2010–2024). Two independent reviewers conducted screening, data extraction, and risk of bias assessment. Due to heterogeneity, findings were synthesized narratively.
Results: Fifteen studies met inclusion criteria. AI models achieved high predictive accuracy in mortality (AUROC >0.92 in traumatic brain injury), sepsis identification, hospital admission, cardiac arrest, and triage in both adults and children. NLP-based systems improved acuity assignment by leveraging unstructured clinical narratives. Consistently, AI outperformed conventional triage tools in sensitivity, efficiency, and early risk recognition. Nonetheless, most studies were retrospective, single-centre, and lacked external validation, limiting generalizability.
Conclusions: AI demonstrates significant potential to advance emergency medicine by strengthening triage and prediction capabilities. To ensure safe translation into practice, future efforts must emphasize prospective multicentre trials, explainable models, and equitable integration into clinical workflows.
Keywords
Artificial Intelligence; Emergency Medicine; Machine Learning; Deep Learning; Natural Language Processing; Emergency Department; Triage; Critical Care; Risk Stratification; Patient Outcomes
Introduction
Artificial intelligence (AI) has emerged as a transformative force across healthcare, with particular promise in time-sensitive fields such as emergency medicine and critical care. The ability to rapidly analyze vast amounts of structured and unstructured data offers clinicians new opportunities to improve diagnostic accuracy, patient triage, and therapeutic decision-making in high-stakes environments (Saqib et al., 2023). Given the dynamic nature of emergency departments (EDs), where rapid recognition and timely intervention can alter outcomes, the integration of AI tools represents both a challenge and an opportunity for modern medicine (Yoon, Pinsky, & Clermont, 2022).
The urgency of care delivery in the ED underscores the importance of efficient decision support. Traditional triage systems, though widely used, may be limited by subjectivity and inter-clinician variability. AI-powered models, particularly those based on machine learning (ML) and deep learning (DL), can leverage electronic health records, physiological signals, and imaging data to augment clinical judgment (Liu, Zhang, Ho, & Ong, 2018). Studies have highlighted that AI-driven triage algorithms often outperform conventional tools, reducing under-triage while maintaining high sensitivity for critical illness (Dhillon, Zhang, Grewal, & Kashyap, 2024).
Beyond triage, AI applications have expanded into predictive analytics for outcomes such as mortality, intensive care admission, and treatment response. For example, neural networks and gradient boosting models have demonstrated high discriminatory performance in predicting adverse events, sometimes exceeding clinician-based scoring systems (Porcellato, Lanera, Ocagli, & Danielis, 2025). These advances suggest that AI has the potential to enhance not only efficiency but also patient safety in environments where delayed recognition can be catastrophic.
Natural language processing (NLP) is another promising frontier, enabling extraction of clinically relevant information from unstructured clinical narratives. Emergency physicians often rely on rapid documentation during patient encounters, and NLP-enhanced algorithms can parse this data to support real-time risk stratification and prognosis (Zhang, Song, & Liu, 2020). Importantly, these tools have shown early promise in tailoring recommendations to specific patient populations, which may help address disparities in emergency care delivery (Topol, 2019).
Despite these encouraging developments, challenges remain in implementing AI in real-world ED workflows. Issues of model generalizability, bias, and transparency raise concerns about safety and equity (Rajpurkar et al., 2022). Furthermore, data heterogeneity across health systems-spanning differences in patient demographics, clinical practices, and documentation styles-can significantly impact algorithm performance (Beam & Kohane, 2018). Overcoming these limitations requires careful model validation, prospective trials, and consideration of ethical implications in AI deployment.
Another barrier to widespread adoption is the integration of AI into clinical decision support systems without disrupting clinician workflows. Studies have emphasized that AI should act as an augmentation rather than replacement of physician expertise (Sendak et al., 2020). Effective implementation demands user-friendly interfaces, clinician trust in algorithm outputs, and clear interpretability of predictions (Tonekaboni, Joshi, McCradden, & Goldenberg, 2019). Failure to address these factors may result in underutilization despite strong algorithmic performance in research settings.
The rapid pace of innovation also raises regulatory and governance questions. Ensuring patient data privacy, addressing potential liability issues, and developing standards for algorithm evaluation are critical for safe deployment in emergency settings (Benjamens, Dhunnoo, & Mesko, 2020). Cross-disciplinary collaboration between clinicians, data scientists, policymakers, and ethicists will therefore be essential in shaping a responsible future for AI in acute care.
Ultimately, the systematic evaluation of AI in emergency medicine is crucial to synthesize existing evidence and identify gaps for future research. By collating findings across diverse clinical contexts, this review aims to clarify the impact of AI tools on patient care, highlight methodological challenges, and provide recommendations for the safe and effective integration of AI into emergency medicine practice.
Methodology
Study Design
This review employed a systematic review methodology, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines to ensure methodological rigor, transparency, and reproducibility. The aim was to synthesize peer-reviewed evidence on the role of artificial intelligence (AI) applications in emergency medicine, with particular focus on patient-centered outcomes such as triage accuracy, mortality prediction, hospital admission forecasting, and detection of critical illness.
Eligibility Criteria
Studies were included based on the following predefined criteria:
- Population: Patients of all ages (adults, paediatrics, and geriatric) presenting to emergency departments (EDs) or critical care settings.
- Interventions/Exposures: Any application of AI, including machine learning (ML), deep learning (DL), and natural language processing (NLP) models, used to support clinical decision-making, triage, outcome prediction, or workflow optimization in ED or urgent care contexts.
- Comparators: Conventional risk scores, standard triage tools, or clinician judgment alone.
- Outcomes: Prediction accuracy (e.g., AUROC, sensitivity, specificity, PPV, NPV), impact on triage or admission decisions, clinical outcomes (e.g., mortality, length of stay, ICU admission), and workflow efficiency.
- Study Designs: Retrospective cohorts, prospective validation studies, case-control studies, cross-sectional analyses, and randomized controlled trials (RCTs) where available.
- Language: Only articles published in English were included.
- Publication Period: 2010 to 2024, ensuring contemporary relevance in line with the evolution of AI methods in healthcare.
Search Strategy
A comprehensive literature search was performed across PubMed, Scopus, Web of Science, Embase, and IEEE Explore to capture both clinical and computationally focused publications. Supplementary searches were conducted in Google Scholar and reference lists of key systematic reviews to identify additional eligible studies.
Boolean operators were used in various combinations with the following keywords:
- (“artificial intelligence” OR “machine learning” OR “deep learning” OR “neural networks” OR “natural language processing”)
- AND (“emergency medicine” OR “emergency department” OR “acute care” OR “critical care” OR “trauma” OR “triage”)
- AND (“prediction” OR “risk stratification” OR “clinical outcomes” OR “mortality” OR “admission”). (Figure 1).
Study Selection Process
All search results were exported to Zotero reference management software, and duplicates were removed. Titles and abstracts were screened independently by two reviewers for relevance. Full-texts of potentially eligible studies were then reviewed in detail. Any disagreements regarding study inclusion were resolved through discussion or, if necessary, adjudication by a third reviewer. The final pool included 15 studies that satisfied all eligibility criteria.
Data Extraction
A standardized data extraction sheet was designed and piloted. From each eligible study, the following data elements were systematically extracted:
- Author(s), year of publication, and country
- Study design and sample size
- Patient population (age, gender, diagnosis, ED context)
- AI model used (e.g., RF, XG Boost, DNN, NLP models)
- Comparator(s) (e.g., conventional triage, clinician judgment)
- Outcomes measured (AUROC, mortality, admission prediction, workflow metrics)
- Key results (including effect sizes, model performance metrics)
- Reported limitations and confounders addressed
Data extraction was performed independently by two reviewers and verified for accuracy by a third reviewer.
Quality Assessment
The risk of bias and study quality were appraised using tools appropriate to study design:
- Newcastle-Ottawa Scale (NOS) for observational cohort and case-control studies.
- Cochrane Risk of Bias 2.0 Tool for randomized controlled trials.
Studies were categorized as low, moderate, or high quality based on criteria including selection methods, comparability of groups, completeness of outcome assessment, and transparency in reporting AI methodology.
Data Synthesis
Due to heterogeneity in AI models, populations, and outcomes, a narrative synthesis was performed. Key patterns were identified in relation to model performance (AUROC ranges, sensitivity/specificity), ED workflow impact, and patient outcomes. Subgroup analyses by age (Pediatric vs adult), outcome type (mortality, admission, interventions), and AI methodology (ML vs DL vs NLP) were also conducted. Effect estimates (e.g., AUROC, accuracy, odds ratios) were reported where available. No formal meta-analysis was conducted due to variability in outcome measures and AI model definitions.
Ethical Considerations
As this study was a secondary synthesis of published data, no new ethical approval or patient consent was required. All included studies were peer-reviewed and assumed to have received ethical clearance from their respective institutions.
Results
Summary and Interpretation of Included Studies on Artificial Intelligence in Emergency Medicine
- Study Designs and Populations
The included studies were predominantly retrospective cohorts, supplemented by prospective validations and case-control analyses. Sample sizes varied considerably, from smaller datasets (e.g., Ivanov et al., 2021: n = 729 encounters) to large-scale nationwide data (e.g., Hwang et al., 2022: n = 2.62 million Pediatric ED visits). Populations spanned adults, children, and trauma-specific cohorts, reflecting wide applicability of AI in different emergency department (ED) settings.
- AI Models and Performance
Machine learning (ML) and deep learning (DL) approaches were the most common, including Random Forest (RF), Gradient Boosting (GB), XGBoost, Logistic Regression (LR), Deep Neural Networks (DNN), and Natural Language Processing (NLP)-based models. Reported AUROCs ranged from 0.82 to 0.99, consistently outperforming conventional triage tools such as ESI, qSOFA, and HEART/GRACE/TIMI risk scores. Notably, Pediatric ED outcomes (Hwang 2022) and critical intervention prediction (Chang 2022) showed exceptionally high AUROC values (>0.94).
- Clinical Utility and ED Impact
Most studies demonstrated improvements in triage accuracy, early identification of critical illness, and enhanced resource allocation. AI tools showed potential to reduce under-triaging, expedite critical interventions, and support risk stratification in time-sensitive emergencies such as traumatic brain injury, sepsis, and cardiac arrest. NLP applications, particularly in Chen (2023) and Ivanov (2021), improved interpretation of narrative notes and acuity assignment.
- Limitations and Generalizability
Several limitations were recurrent: single-centre settings (e.g., Wu 2021, Chang 2022), exclusion of comorbidities or imaging data (Hsu 2021, Tu 2022), and reliance on retrospective validation without real-time clinical deployment (Xiao 2023, Chen 2023). Performance heterogeneity across populations highlights the need for multi-centre validation, prospective implementation, and consideration of local practice variability (Table 1).
| Author/ Year | Purpose | Study Design | Sample | Quantitative Results (AUC etc.) | ED Effect | |
|---|---|---|---|---|---|---|
| Limitations | ||||||
| Hsu 2021 | Predict in-hospital mortality in TBI patients | Retrospective cohort | 3,331 TBI patients, Taiwan | RF (0.921), J48 (0.82), NB (0.917), REP tree (0.846) | Improved prognosis awareness and early risk stratification | Single site, no comorbidities or imaging considered |
| Hwang 2022 | Predict critical illness & hospitalization in children visiting ED | Retrospective cohort | 2,621,710 children <15 yrs, Korea | RF AUROC: 0.991 (critical), 0.943 (hospitalization) | Outperformed conventional triage for pediatric ED | Imbalanced dataset, lower AUPRC |
| Joseph 2020 | Identify critically ill patients at triage using limited info | Retrospective cross-sectional | 445,925 adults, US | NN (0.851), XGBoost (0.82), LR (0.805) | Improved early recognition at triage | Single center, ICU admission criteria variable |
| Liu 2021 | Develop & validate ML triage algorithm | Retrospective + prospective | 22,272 adults, Singapore | CatBoost (0.875), LR (0.843) | Improved triage efficiency | Features like arrival time may vary |
| Raita 2019 | Predict ED outcomes at triage | Retrospective cohort | 135,470 adults, US NHAMCS survey | DNN (0.86), GB (0.85); Hospitalization: DNN (0.82), GB (0.82) | Reduced under-triaging | Thresholds vary, missing data |
| Ivanov 2021 | Improve ESI acuity assignment with ML + NLP | Retrospective | 729 encounters from 147,052 records, US | KATE™ accuracy 75.7% vs nurses 59.8% | More accurate ESI classification | Dependent on nurse baseline |
| Xiao 2023 | Predict severity & specialty allocation | Retrospective | 308,834 ED visits, China | TransNet AUC 0.93, TextRNN 0.98 | Reduced over-/under-triage | Retrospective only |
| Chen 2023 | Use narratives for outcome prediction | Retrospective cohort | 171,275 ED patients, Taiwan | DNN model AUC 0.874 | Outperformed physicians & ML baselines | Missing free-text data, single-site |
| Fernandes 2020 | Predict mortality & arrest with ML + NLP | Retrospective | 235,826 ED visits, Portugal | XGBoost (0.96), LR (0.95), RF (0.94) | Improved triage sensitivity (MTS-3) | Excluded nonurgent patients |
| Tu 2022 | AI system for TBI mortality risk | Retrospective | 18,249 TBI patients, Taiwan | LR (0.925), XGBoost (0.871), RF (0.87) | Early mortality prediction | No imaging/labs, limited generalizability |
| Chang 2022 | Suggest critical interventions at triage | Retrospective observational | 137,883 adults, Korea | Intubation 0.945, transfusion 0.920, oxygen 0.909 | High accuracy, reduced delays | Single-center |
| Lin 2021 | Identify sepsis in ED patients | Retrospective cohort | 8,296 adults, Taiwan | GB (0.86), XGBoost PPV 0.47 / NPV 0.94 | Outperformed qSOFA & SIRS | Dataset heterogeneity |
| Lu 2023 | Predict in-hospital cardiac arrest at ED | Retrospective | 316,465 ED patients, Taiwan | RF (0.931), GB (0.93), LR (0.905) | Early identification of cardiac arrest | Single hospital |
| Hong 2018 | Predict hospital admission at triage | Retrospective | 202,953 adults, 3 EDs, Yale US | XGBoost (0.924), DNN (0.920), LR (0.909) | Admission prediction feasible | Doesn’t address implementation barriers |
| Wu 2021 | Predict critical outcomes in chest pain | Retrospective case-control | 3,146 chest pain patients, China | LASSO regression (0.953) | Outperformed HEART, GRACE, TIMI | Case-control limits generalizability |
Discussion
The findings of this systematic review demonstrate the growing influence of artificial intelligence (AI) in emergency medicine, where timely and accurate decisions are critical for patient outcomes. AI models across multiple studies consistently demonstrated strong discriminatory performance, often outperforming conventional triage tools and clinical judgment alone. For example, deep learning approaches in triage and outcome prediction (Joseph et al., 2020; Chen et al., 2023) surpassed traditional models, highlighting AI’s ability to extract subtle, nonlinear patterns from complex data streams in emergency department (ED) settings.
AI applications in triage remain a key area of advancement. Several studies showed that machine learning algorithms could significantly improve risk stratification and reduce under-triaging in both adult and Pediatric populations (Raita et al., 2019; Hwang & Lee, 2022; Wolff, Rios, & Grana, 2019). These results are consistent with broader reviews emphasizing the ability of AI to enhance rapid decision-making in acute care (Liu, Zhang, Ho, & Ong, 2018; Yoon, Pinsky, & Clermont, 2022). Importantly, AI-based triage tools may mitigate subjective variation inherent in traditional triage systems, increasing consistency and reliability across clinicians and institutions.
Beyond triage, AI has demonstrated value in predicting critical outcomes, including mortality, sepsis, and cardiac arrest. Hsu et al. (2021) and Tu et al. (2022) reported accurate mortality prediction in traumatic brain injury patients using machine learning, while Lin et al. (2021) showed that gradient boosting outperformed established sepsis tools such as qSOFA. Similarly, Lu et al. (2023) developed models to predict in-hospital cardiac arrest with AUROC values exceeding 0.93, underscoring AI’s potential to identify deteriorating patients early. These findings align with the broader argument that AI can extend the diagnostic and prognostic capabilities of emergency clinicians (Saqib, Iftikhar, Neha, Karishma, & Mumtaz, 2023).
Several studies extended AI’s reach to specific conditions and populations. Wu et al. (2021) demonstrated that AI models could outperform traditional risk scores in predicting outcomes among chest pain patients, while Goto et al. (2018) and Patel, Chamberlain, and Chamberlain (2018) reported strong predictive accuracy for asthma and COPD exacerbations in the ED. Levartovsky et al. (2021) highlighted AI’s ability to predict intra-abdominal abscesses in Crohn’s disease patients. These targeted applications illustrate AI’s adaptability across diverse emergency presentations and its promise for precision medicine in acute care.
Natural language processing (NLP) emerged as a powerful complement to structured data, enabling real-time use of free-text narratives. Chen et al. (2023) and Ivanov et al. (2021) demonstrated that NLP-enhanced models improved acuity assignment and outcome prediction compared with clinician assessments. Fernandes et al. (2020) further showed that combining machine learning with NLP significantly improved mortality prediction in Portuguese EDs. These findings reflect broader enthusiasm about NLP’s potential to unlock unstructured data sources, which are abundant in ED documentation (Zhang, Song, & Liu, 2020).
AI has also been shown to support clinical interventions and workflow optimization. Chang et al. (2022) demonstrated that machine learning could accurately recommend timely interventions such as intubation and transfusion, potentially reducing delays in critical care delivery. Lee et al. (2022) used AI to personalize length of stay predictions for syncope patients, improving bed management and discharge planning. Feretzakis et al. (2022) and Hong, Haimovich, and Taylor (2018) confirmed the feasibility of predicting admission risk early in triage, which has important implications for ED crowding and resource allocation. These innovations align with global calls for AI to enhance efficiency without compromising safety (Topol, 2019).
Despite encouraging performance metrics, several limitations temper the generalizability of current AI models. Most studies were retrospective, often based on single-center data, which risks overfitting and reduces external validity (Chang et al., 2022; Chen et al., 2023). Variations in inclusion criteria, outcome definitions, and input variables further contribute to heterogeneity, making direct comparison challenging (Beam & Kohane, 2018). Additionally, as Rajpurkar, Chen, Banerjee, and Topol (2022) caution, lack of transparency in AI model development and limited explain ability may undermine clinician trust and adoption.
The issue of explain ability is particularly salient in emergency medicine, where clinicians must make high-stakes decisions rapidly. Black-box models such as deep neural networks may yield impressive accuracy but offer limited interpretability. Efforts to contextualize explainability for clinical use (Tonekaboni, Joshi, McCradden, & Goldenberg, 2019) suggest that clinician-friendly explanations are essential for adoption. Sundrani et al. (2023), for example, highlighted the importance of transparency when deploying continuous physiologic monitoring systems that predict patient decompensation. Without explainability, clinicians may hesitate to rely on algorithmic recommendations, limiting potential impact.
Integration into real-world workflows remains another barrier. Sendak et al. (2020) emphasized that AI should augment, not replace, clinician judgment. Studies such as Ivanov et al. (2021) and Klang et al. (2021) show how AI can complement traditional triage by adding decision support layers, but seamless integration into electronic health records and user-friendly interfaces remains underdeveloped. As Porcellato, Lanera, Ocagli, and Danielis (2025) observed in critical care nursing, aligning AI with clinician workflows is essential to prevent added burden or resistance.
Regulatory oversight and safety assurance are additional concerns. Benjamens, Dhunnoo, and Mesko (2020) catalogued the rise of FDA-approved AI algorithms in healthcare, but most have limited application in emergency medicine. Emergency care poses unique challenges such as heterogeneous populations, rapid turnover, and high-risk decision points, making rigorous validation even more critical. Failure to address these factors risks unsafe deployment and could exacerbate inequities if models underperform in underrepresented populations.
Ethical considerations also loom large. AI models trained on biased data may inadvertently perpetuate disparities in care (Rajpurkar et al., 2022). For instance, differences in triage accuracy across Pediatric and adult populations (Hwang & Lee, 2022; Patel et al., 2018) highlight the risk of uneven performance. Equity-focused validation across demographic subgroups is therefore essential. Moreover, privacy concerns regarding sensitive ED data require robust safeguards, as highlighted in discussions on AI governance in healthcare (Saqib et al., 2023).
From a methodological perspective, the review highlights the need for multicentre prospective trials to confirm external validity. While studies such as Liu et al. (2021) and Lu et al. (2023) provided strong validation within specific settings, broad implementation requires testing across varied healthcare systems. Standardization of reporting and benchmarking, as advocated by Wolff et al. (2019), would also facilitate cross-study comparison and accelerate responsible innovation.
Looking ahead, hybrid models combining structured data, continuous monitoring, and unstructured narratives hold particular promise. For example, Sundrani et al. (2023) demonstrated the utility of physiologic data streams, while Chen et al. (2023) leveraged narratives, and Wu et al. (2021) used condition-specific inputs. Integrating these modalities could yield more robust, generalizable tools. Furthermore, cross-disciplinary collaboration between clinicians, engineers, ethicists, and policymakers is critical to move from pilot studies to safe clinical deployment (Dhillon, Zhang, Grewal, & Kashyap, 2024).
Finally, AI’s transformative potential in emergency medicine is underscored by its ability to reshape traditional paradigms of acute care delivery. As Topol (2019) and Saqib et al. (2023) argue, the convergence of human expertise with AI-driven insights heralds a new era of high-performance medicine. To fully realize this vision, future efforts must balance accuracy with interpretability, innovation with regulation, and efficiency with equity. By addressing these challenges, AI has the potential to meaningfully improve patient care in emergency and critical care medicine.
Conclusion
This systematic review underscores the transformative potential of AI in emergency medicine, particularly in enhancing triage accuracy, predicting critical illness, and improving workflow efficiency. Across multiple applications, AI consistently outperformed traditional scoring systems and clinician-only assessments, supporting its role as a powerful tool for augmenting acute care decision-making. The incorporation of NLP further expands AI’s capacity by leveraging unstructured clinical narratives, addressing a long-standing gap in emergency data utilization.
Despite these promising findings, significant barriers remain before AI can be fully embedded into clinical practice. Most existing studies are retrospective, with limited external validity and insufficient assessment of equity, interpretability, and integration into real-time ED workflows. To translate algorithmic success into patient-centered impact, future research must prioritize multicentre prospective trials, regulatory oversight, and the development of transparent, clinician-friendly models. Achieving these goals will be critical to realizing AI’s potential for safer, more efficient, and equitable emergency medicine.
References
Benjamens, S., Dhunnoo, P., & Mesko, B. (2020). The state of artificial intelligence-based FDA-approved medical devices and algorithms: An online database. npj Digital Medicine, 3, 118.
Beam, A. L., & Kohane, I. S. (2018). Big data and machine learning in health care. JAMA, 319(13), 1317–1318.
Chang, H., Yu, J. Y., Yoon, S., Kim, T., & Cha, W. C. (2022). Machine learning-based suggestion for critical interventions in the management of potentially severe conditioned patients in emergency department triage. Scientific Reports, 12, 10537.
Chen, M. C., Huang, T. Y., Chen, T. Y., Boonyarat, P., & Chang, Y. C. (2023). Clinical narrative-aware deep neural network for emergency department critical outcome prediction. Journal of Biomedical Informatics, 138, 104284.
Choi, D. H., Hong, K. J., Park, J. H., et al. (2022). Prediction of bacteremia at the emergency department during triage and disposition stages using machine learning models. American Journal of Emergency Medicine, 53, 86–93.
Dhillon, G., Zhang, Z., Grewal, H., & Kashyap, R. (2024). Clinical application of artificial intelligence in emergency and critical care medicine, volume IV. Frontiers in Medicine, 10, 1346070.
Feretzakis, G., Karlis, G., Loupelis, E., et al. (2022). Using machine learning techniques to predict hospital admission at the emergency department. Journal of Critical Care Medicine (Targu Mures), 8, 107–116.
Fernandes, M., Mendes, R., Vieira, S. M., et al. (2020). Risk of mortality and cardiopulmonary arrest in critical patients presenting to the emergency department using machine learning and natural language processing. PLoS One, 15, e0230876.
Goto, T., Camargo, C. A., Faridi, M. K., Yun, B. J., & Hasegawa, K. (2018). Machine learning approaches for predicting disposition of asthma and COPD exacerbations in the ED. American Journal of Emergency Medicine, 36, 1650–1654.
Hong, W. S., Haimovich, A. D., & Taylor, R. A. (2018). Predicting hospital admission at emergency department triage using machine learning. PLoS One, 13, e0201016.
Hsu, S. D., Chao, E., Chen, S. J., Hueng, D. Y., Lan, H. Y., & Chiang, H. H. (2021). Machine learning algorithms to predict in-hospital mortality in patients with traumatic brain injury. Journal of Personalized Medicine, 11, 1144.
Hwang, S., & Lee, B. (2022). Machine learning-based prediction of critical illness in children visiting the emergency department. PLoS One, 17, e0264184.
Ivanov, O., Wolf, L., Brecher, D., et al. (2021). Improving ED Emergency Severity Index acuity assignment using machine learning and clinical natural language processing. Journal of Emergency Nursing, 47, 265–278.e7.
Joseph, J. W., Leventhal, E. L., Grossestreuer, A. V., et al. (2020). Deep-learning approaches to identify critically ill patients at emergency department triage using limited information. Journal of the American College of Emergency Physicians Open, 1, 773–781.
Klang, E., Kummer, B. R., Dangayach, N. S., et al. (2021). Predicting adult neuroscience intensive care unit admission from emergency department triage using a retrospective, tabular-free text machine learning approach. Scientific Reports, 11, 1381.
Lee, S., Mudireddy, A. R., Pasupula, D. K., et al. (2022). Novel machine learning approach to predict and personalize length of stay for patients admitted with syncope from the emergency department. Journal of Personalized Medicine, 13, 7.
Levartovsky, A., Barash, Y., Ben-Horin, S., et al. (2021). Machine learning for prediction of intra-abdominal abscesses in patients with Crohn’s disease visiting the emergency department. Therapeutic Advances in Gastroenterology, 14, 17562848211053114.
Lin, P. C., Chen, K. T., Chen, H. C., Islam, M. M., & Lin, M. C. (2021). Machine learning model to identify sepsis patients in the emergency department: Algorithm development and validation. Journal of Personalized Medicine, 11, 1055.
Liu, N., Zhang, Z., Ho, A. F. W., & Ong, M. E. H. (2018). Artificial intelligence in emergency medicine. Journal of Emergency and Critical Care Medicine, 2, 82.
Liu, Y., Gao, J., Liu, J., et al. (2021). Development and validation of a practical machine-learning triage algorithm for the detection of patients in need of critical care in the emergency department. Scientific Reports, 11, 24044.
Lu, T. C., Wang, C. H., Chou, F. Y., et al. (2023). Machine learning to predict in-hospital cardiac arrest from patients presenting to the emergency department. Internal and Emergency Medicine, 18, 595–605.
Pai, D. R., Rajan, B., Jairath, P., & Rosito, S. M. (2023). Predicting hospital admission from emergency department triage data for patients presenting with fall-related fractures. Internal and Emergency Medicine, 18, 219–227.
Patel, S. J., Chamberlain, D. B., & Chamberlain, J. M. (2018). A machine learning approach to predicting need for hospitalization for pediatric asthma exacerbation at the time of emergency department triage. Academic Emergency Medicine, 25, 1463–1470.
Porcellato, E., Lanera, C., Ocagli, H., & Danielis, M. (2025). Exploring applications of artificial intelligence in critical care nursing: A systematic review. Nursing Reports, 15(2), 55.
Raita, Y., Goto, T., Faridi, M. K., Brown, D. F., Camargo, C. A., & Hasegawa, K. (2019). Emergency department triage prediction of clinical outcomes using machine learning models. Critical Care, 23, 64.
Rajpurkar, P., Chen, E., Banerjee, O., & Topol, E. J. (2022). AI in health and medicine. Nature Medicine, 28(1), 31–38.
Saqib, M., Iftikhar, M., Neha, F., Karishma, F., & Mumtaz, H. (2023). Artificial intelligence in critical illness and its impact on patient care: A comprehensive review. Frontiers in Medicine, 10, 1176192.
Sendak, M. P., D’Arcy, J., Kashyap, S., Gao, M., Nichols, M., Corey, K., & Balu, S. (2020). A path for translation of machine learning products into healthcare delivery. EMJ Innovations, 4(1), 9–15.
Sundrani, S., Chen, J., Jin, B. T., Abad, Z. S. H., Rajpurkar, P., & Kim, D. A. (2023). Predicting patient decompensation from continuous physiologic monitoring in the emergency department. Academic Emergency Medicine, 60, 6.
Tonekaboni, S., Joshi, S., McCradden, M. D., & Goldenberg, A. (2019). What clinicians want: Contextualizing explainable machine learning for clinical end use. Machine Learning for Healthcare Conference, 20, 359–380.
Topol, E. J. (2019). High-performance medicine: The convergence of human and artificial intelligence. Nature Medicine, 25(1), 44–56.
Tu, K. C., Nyam, T. T., Wang, C. C., et al. (2022). A computer-assisted system for early mortality risk prediction in patients with traumatic brain injury using artificial intelligence algorithms in emergency room triage. Brain Sciences, 12, 612.
Wolff, P., Rios, S. A., & Grana, M. (2019). Setting up standards: A methodological proposal for pediatric triage machine learning model construction based on clinical outcomes. Expert Systems with Applications, 138, 112792.
Wu, T. T., Zheng, R. F., Lin, Z. Z., Gong, H. R., & Li, H. (2021). A machine learning model to predict critical care outcomes in patients with chest pain visiting the emergency department. BMC Emergency Medicine, 21, 112.
Xiao, Y., Zhang, J., Chi, C., Ma, Y., & Song, A. (2023). Criticality and clinical department prediction of ED patients using machine learning based on heterogeneous medical data. Computers in Biology and Medicine, 165, 107390.
Yoon, J. H., Pinsky, M. R., & Clermont, G. (2022). Artificial intelligence in critical care medicine. Annual Update in Intensive Care and Emergency Medicine 2022, 353–367.
Zhang, Y., Song, J., & Liu, X. (2020). Natural language processing in emergency medicine: Applications and challenges. BMC Medical Informatics and Decision Making, 20, 253.