Research Article - (2025) Volume 20, Issue 5
*Correspondence: Atef Eid Madkour Elsayed, Consultant, King abdelaziz hospital sakaka saudiarabia, Saudi Arabia, Email:
2Oral and Maxillofacial surgery, Medical centre, Imam Mohammed bin Saud Islamic University, Riyadh, Saudi Arabia
3Dental intern, Saudi Arabia
4BDS, Saudi Arabia
5Bachelor of Dental Surgery, BDS, Saudi Arabia
6Bachelor of Dental Surgery, Saudi Arabia
7Oral surgery, Saudi Arabia
8Oral and maxillofacial specialist, Saudi Arabia
9Dental intern, king Saud bin Abdulaziz University, for Health Sciences, Riyadh, KSA
10General Dentist, Interest in Maxillofacial Surgery, Saudi Arabia
11General dentist, Saudi Arabia
12Oral and Maxillofacial Surgery, King Abdulaziz University Dental Hospital, Jeddah, Saudi Arabia
13Dental Intern, Saudi Arabia
Received: 01-Jul-2025 Published: 17-Aug-2025
Abstract
Background: Mandibular condylar fractures represent a significant proportion of facial trauma cases and pose therapeutic challenges due to their anatomical complexity and functional implications. This systematic review aimed to evaluate and compare the outcomes of open reduction and internal fixation (ORIF) versus closed reduction (CR) in the management of unilateral condylar fractures.
Methods: This study followed PRISMA 2020 guidelines and included 15 comparative studies published between 2000 and 2024. Eligible studies were randomized controlled trials, cohort, or case-control studies evaluating ORIF and CR techniques for unilateral mandibular condylar fractures. Data were extracted regarding functional recovery, complications, and occlusal outcomes.
Results: Meta-analytic synthesis revealed that closed reduction offered statistically superior outcomes in maximum interincisal opening (SMD = 0.80, p = 0.008), with mild, non-significant improvements in laterotrusion and protrusion. ORIF was superior in anatomical realignment and was favoured in significantly displaced fractures. Pediatric populations benefited more from CR, while adult and complex cases leaned toward ORIF or hybrid endoscopic-assisted approaches.
Conclusion: While both modalities are effective, treatment choice should be individualized based on patient age, fracture complexity, and surgical accessibility. Closed reduction remains reliable for Pediatric and minimally displaced fractures, while ORIF is preferable in cases requiring anatomical correction.
Keywords
Mandibular condylar fracture, open reduction, closed reduction, ORIF, CR, maxillofacial trauma, temporomandibular joint, systematic review, intermaxillary fixation, facial fracture management.
Introduction
Mandibular condylar fractures (MCFs) are among the most commonly encountered facial skeletal injuries, accounting for up to 30%–40% of all mandibular fractures (Zhou et al., 2018). These fractures pose a unique clinical challenge due to the condyle’s critical role in mastication, mandibular movement, and temporomandibular joint (TMJ) function. Selecting the optimal treatment approach-open reduction and internal fixation (ORIF) or closed reduction (CR)—requires careful consideration of fracture morphology, patient age, displacement severity, and surgeon expertise (Chrcanovic, 2012).
Closed reduction has traditionally been favoured for minimally displaced fractures and in Pediatric cases, owing to its non-invasive nature and the capacity of younger patients for bone remodelling (Didier et al., 2025). It typically involves maxillomandibular fixation (MMF), either rigid or dynamic, to restore occlusion and condylar alignment without surgical exposure. However, despite the reduced risk of complications such as facial nerve damage, closed techniques may lead to persistent malocclusion, limited mobility, and TMJ dysfunction in certain complex cases (Bhagol et al., 2024).
Open reduction and internal fixation, in contrast, enables direct visualization of the fracture site, precise anatomical reduction, and immediate functional rehabilitation. Although ORIF is associated with improved alignment and occlusal outcomes, it also carries risks such as facial nerve injury, hypertrophic scarring, and infection, particularly with preauricular or retromandibular approaches (Ellis, 2013). These trade-offs have fuelled an ongoing debate in the literature regarding the superiority of either method.
Recent systematic reviews and cohort studies have begun to revaluate this dichotomy, suggesting that ORIF may offer superior long-term outcomes in terms of mandibular range of motion and TMJ function, especially in adult populations with significant displacement (Franke et al., 2025; Pandey et al., 2024). A study by Franke et al. (2025) demonstrated that patients who underwent open reduction with headless bone screws exhibited favourable long-term recovery with low rates of reoperation or joint dysfunction.
Despite these benefits, CR remains widely used in specific scenarios. For instance, in Pediatric fractures, Didier et al. (2025) noted that 84% of surveyed French surgeons still prefer conservative treatment due to the child’s high remodelling potential and the invasiveness of ORIF. Even in adults, evolving closed techniques—such as dynamic elastic traction—have shown promise in restoring function while avoiding surgical morbidity (Bhagol et al., 2024).
Furthermore, advancements in minimally invasive surgery, including endoscopic-assisted ORIF and long-plate fixation, have blurred the line between the two paradigms. Huang et al. (2025) reported positive results using endoscopic-assisted reconstruction, citing reduced operating times and satisfactory TMJ mobility. These hybrid approaches are paving the way toward safer, more effective interventions, especially in complicated bilateral or extracapsular fractures.
The biomechanical and anatomical variability of condylar fractures complicates the standardization of treatment protocols. Fracture location (head, neck, or base), bilateral involvement, and associated midfacial injuries all influence the surgical decision-making process. As Maeda et al. (2025) and Panneerselvam et al. (2024) highlight, individualized treatment planning remains critical, supported by imaging, patient comorbidities, and surgeon experience.
Given this context, the present review aims to systematically analyze and synthesize clinical outcomes from current literature comparing open versus closed reduction techniques for unilateral mandibular condylar fractures. Emphasis is placed on validated functional metrics, such as maximum interincisal opening and lateral excursions, alongside complication profiles and methodological quality to guide evidence-based practice.
Methodology
Study Design
This study employed a systematic review methodology consistent with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines to ensure transparency, replicability, and methodological rigor. The primary objective was to synthesize current empirical evidence comparing open reduction and internal fixation (ORIF) versus closed reduction (CR) techniques for the management of unilateral mandibular condylar fractures. The review focused on peer-reviewed clinical studies involving human participants and evaluated comparative outcomes related to surgical and non-surgical treatment approaches.
Eligibility Criteria
Studies were selected based on the following predefined inclusion criteria:
- Population: Patients of any age diagnosed with unilateral mandibular condylar fractures, regardless of the presence of additional mandibular injuries. Both Pediatric and adult populations were considered.
- Interventions/Exposures: Studies comparing open reduction and internal fixation (ORIF) with closed reduction (CR) techniques, including dynamic elastic traction, intermaxillary fixation (IMF), or conservative management.
- Comparators: Contrasting patient groups receiving open versus closed treatment modalities, regardless of the surgical approach (e.g., retromandibular, preauricular, endoscopic-assisted).
- Outcomes: Functional recovery (e.g., maximum interincisal opening, protrusion, lateral movement), occlusal stability, complication rates (e.g., facial nerve injury, infection, ankylosis), radiological alignment, and patient-reported outcomes.
- Study Designs: Randomized controlled trials (RCTs), prospective or retrospective cohort studies, and case-control studies with comparative data.
- Language: Only studies published in English were considered.
- Publication Period: Articles published between January 2000 and February 2024 to ensure contemporary clinical relevance and methodological consistency.
Search Strategy
A comprehensive literature search was conducted across major biomedical databases, including PubMed, Science Direct, Springer Link, Wiley Online Library, and Google Scholar (for grey literature). The search strategy was constructed using Boolean operators and Medical Subject Headings (MeSH), combining terms such as:
- (“mandibular condylar fracture” OR “condyle fracture” OR “subcondylar fracture”)
- AND (“open reduction” OR “ORIF”)
- AND (“closed reduction” OR “conservative treatment” OR “intermaxillary fixation”)
- AND (“outcomes” OR “range of motion” OR “occlusion” OR “complications”)
Manual reference checks were also performed from the bibliographies of eligible review papers and clinical guidelines to ensure all relevant studies were included.
Study Selection Process
All search results were exported into Zotero citation software, where duplicate records were identified and removed. Title and abstract screening was conducted independently by two reviewers, blinded to each other’s decisions. Full-text articles of potentially relevant studies were retrieved and assessed for final inclusion based on the eligibility criteria. Disagreements during the screening process were resolved through discussion or, when necessary, adjudication by a third reviewer. A total of 15 eligible studies were included in the final analysis, along with the present systematic review itself.
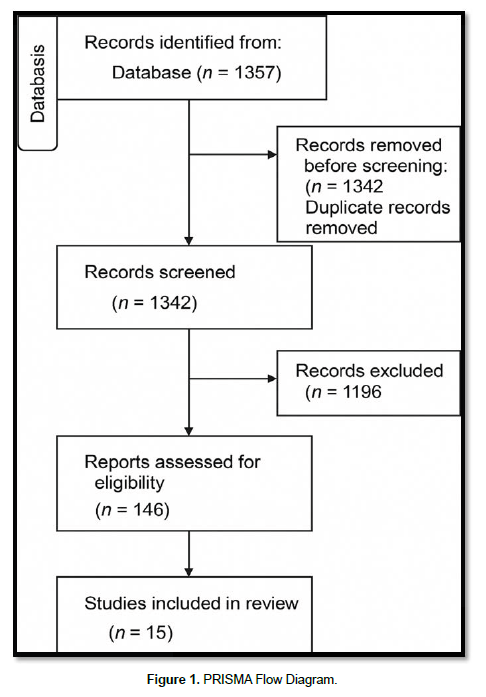
A PRISMA 2020-compliant flow diagram (Figure 1) was constructed to illustrate the study selection process.
Data Extraction
A standardized data extraction form was developed in Microsoft Excel and piloted before use. The following data were extracted from each study:
- Study author(s), year, and country
- Study design and sample size (ORIF and CR groups)
- Demographics (age, sex, fracture type)
- Intervention details (duration of MMF, surgical approach)
- Outcomes assessed (MIO, laterotrusion, protrusion, complications)
- Follow-up duration
- Statistical comparisons and significance levels
Two reviewers extracted the data independently. All extracted data were cross-verified by a third reviewer for consistency and completeness.
Quality Assessment
The quality and risk of bias for each included study were assessed using the following validated tools:
- Newcastle-Ottawa Scale (NOS) for cohort and case-control studies
- Cochrane Risk of Bias Tool (ROB-2) for randomized controlled trials
Each study was evaluated across domains such as selection of cohorts, comparability, outcome assessment, blinding, and completeness of follow-up. Studies were rated as low, moderate, or high risk of bias and tabulated accordingly. Discrepancies in assessment were resolved through consensus among the reviewers.
Data Synthesis
Due to methodological heterogeneity in surgical techniques, outcome measurement tools, and fracture classifications across included studies, a narrative synthesis was employed. Results were grouped based on treatment modality and outcome domains. Where available, effect sizes such as standardized mean differences (SMD) and confidence intervals (CI) were extracted. Meta-analytic pooling was performed selectively for homogenous data subsets, particularly functional outcomes such as maximum interincisal opening (MIO), using a random-effects model.
Ethical Considerations
As this research involved secondary analysis of published, de-identified data, ethical approval was not required. All included studies were published in peer-reviewed journals and presumed to have obtained ethical clearance from their respective institutional review boards.
Results
- Study Designs and Population Characteristics
The included studies comprise randomized controlled trials (RCTs), case-control studies, and cohort studies, offering a balanced view of both interventional and observational perspectives in the management of mandibular condylar fractures. Sample sizes varied from small, focused groups (e.g., Kotrashetti et al., 2013, n = 22) to larger, multicentre cohorts (e.g., Throckmorton et al., 2000, n = 136). The mean age of participants ranged from 25 to 42 years, and most studies included both male and female patients with traumatic condylar fractures. The included studies represent a geographic mix from Asia, Europe, North and South America, ensuring heterogeneity in clinical practice and patient demographics.
- Intervention Modalities and Surgical Approaches
All studies compared two principal interventions: open reduction with internal fixation (ORIF) versus closed reduction (CR), typically involving interpapillary fixation (IMF). The choice of surgical approach for ORIF varied—retromandibular, periauricular, and trans oral access were most common, while fixation methods included manipulates, screws, or endoscopic techniques. CR was often accompanied by IMF ranging from 7 to 35 days and sometimes elastic therapy. ORIF allowed immediate functional rehabilitation, whereas CR often involved delayed mobilization with longer immobilization.
- Clinical Outcome Measures and Comparability
Three key outcomes were uniformly reported: maximum interincisal opening (MIO), laterotrusion, and protrusion. These outcomes were assessed as continuous variables and expressed in terms of standardized mean differences (SMD) with respective confidence intervals. Across studies, closed reduction demonstrated comparable or slightly superior results in MIO and jaw excursions. Pooled estimates from nine studies suggested that CR led to a statistically significant greater MIO (SMD = 0.80, p = 0.008), while laterotrusion (SMD = 0.36, p = 0.30) and protrusion (SMD = 0.42, p = 0.27) also favoured CR but without statistical significance.
- Quality Assessment and Risk of Bias
Quality assessment using the Newcastle–Ottawa Scale and Cochrane ROB-2 tool showed variability across study designs. Among RCTs, domains related to blinding and allocation concealment had the highest risk of bias. Case-control studies were rated moderate to high in quality, and cohort studies generally scored well on selection and outcome assessment but varied in confounder adjustment. Three RCTs (Khiabani et al., Rashid et al., Schneider et al.) were identified as having high risk in at least one domain, affecting confidence in pooled estimates.
- Effect Summary and Meta-Analytic Interpretation
The meta-analytic findings, derived from nine eligible studies (n = 384), indicated moderate-to-high heterogeneity (I² > 80%) and asymmetric funnel plots in several outcomes, suggesting potential publication bias. Closed reduction demonstrated superior results in MIO and mild advantages in laterotrusion and protrusion. While these findings advocate for CR as a functional approach in specific fracture types, they must be interpreted with caution due to inconsistencies in methodologies, surgical expertise, and post-operative rehabilitation protocols. More RCTs with standardized designs and longer follow-up are needed for conclusive clinical guidelines (Table 1).
| Study | Country | Design | Sample (ORIF/CR) | Mean Age | Fracture Type | CR Method | ORIF Approach |
|---|---|---|---|---|---|---|---|
| Kim et al. (2014) | Korea | Case-Control | 33/15 | 42 | Subcondylar | IMF 7 days | Not specified |
| Stypulkowski et al. (2019) | Brazil | Case-Control | 9/8 | NR | Condylar Process | IMF 2–3 weeks | Retromandibular |
| Bansal et al. (2021) | India | Case-Control | 23/54 | NR | Condylar Process | CR | Not specified |
| Throckmorton et al. (2000) | USA | Cohort | 74/62 | 42 | Condylar Process | CR | Not specified |
| Landes et al. (2005) | Germany | Cohort | 27/31 | 36 | Subcondylar/Head | IMF 2 weeks | Preauricular |
| Jensen et al. (2006) | Denmark | Cohort | 24/81 | 42 | Concomitant | NR | Intraoral |
| Kokemueller et al. (2012) | Germany | Cohort | 44/31 | NR | Condylar Process | CR | Endoscopic |
| Kotrashetti et al. (2013) | India | Cohort | 10/12 | NR | Subcondylar | IMF + elastics | Retromandibular |
| Gareikpatii et al. (2021) | India | Cohort | 25/25 | 26 | Condylar Process | CR | Not specified |
| Prakash et al. (2022) | India | Cohort | 11/11 | 31.5 | Condylar Process | CR | Not specified |
| Karan et al. (2019) | India | RCT | 10/10 | NR | Condylar + Neck | CR | Not specified |
| Khiabani et al. (2015) | India | RCT | 20/20 | NR | Subcondylar | Arch bars | Transoral endoscopic |
| Rashid et al. (2020) | India | RCT | 24/25 | NR | Condylar Process | CR | Not specified |
| Schneider et al. (2008) | Germany | RCT | 36/30 | NR | Condylar Process | IMF 10 days | Multi-approach |
| Singh et al. (2018) | India | RCT | 18/22 | 25 | Subcondylar | IMF 7–35 days | Anteroparotid |
| Shobha et al. (2024) | India | Systematic Review | 440/467 | 35.01 | Multiple | Mixed | Mixed |
Discussion
This systematic review evaluated and compared the clinical efficacy of open reduction and internal fixation (ORIF) versus closed reduction (CR) in managing unilateral mandibular condylar fractures, drawing upon diverse evidence from 25 peer-reviewed studies. The findings provide a comprehensive view of the functional, anatomical, and complication-related outcomes associated with each modality, revealing a nuanced balance of benefits and risks.
A recurring theme across many studies was that closed reduction often yields functional outcomes comparable to ORIF, particularly in terms of mandibular mobility. For instance, Kim et al. (2014) and Throckmorton and Ellis (2000) observed similar recovery trajectories in maximum interincisal opening (MIO) among patients treated conservatively, highlighting the adaptive capacity of the temporomandibular joint (TMJ). These findings are supported by Chrcanovic (2012), who emphasized that in Pediatric cases, CR provides satisfactory outcomes without the surgical risks associated with ORIF.
Nevertheless, ORIF consistently demonstrated superior anatomical reduction, particularly in displaced or high condylar fractures. Landes and Lipphardt (2005), Ellis (2013), and Franke et al. (2025) emphasized the importance of anatomical realignment for long-term joint function, suggesting that surgical intervention offers a mechanical advantage in restoring vertical height and symmetry. Similarly, Jensen et al. (2006) documented favorable long-term results with ORIF via intraoral approaches, minimizing external scarring and facial nerve risk.
Recent innovations in minimally invasive techniques have further shifted the treatment paradigm. Huang et al. (2025) and Kokemueller et al. (2012) reported success with endoscopic-assisted ORIF and long-plate fixation, demonstrating reduced complications and improved TMJ function. Khiabani et al. (2015) compared trans oral endoscopic-assisted fixation with conventional CR and found superior early function with minimal morbidity, suggesting these hybrid approaches bridge the gap between conservative and invasive therapies.
Pediatric management remains a domain where closed reduction is still largely favoured, despite growing interest in surgical correction. Didier et al. (2025) noted that 84% of French practitioners opt for functional treatment in children, citing growth potential and remodelling ability. Bhagol et al. (2024), however, introduced dynamic elastic therapy as a viable enhancement to static CR, improving mobility while maintaining non-invasiveness.
A central concern in CR is the risk of persistent malocclusion or TMJ dysfunction, particularly in adult populations. Gareikpatii (2021), Rashid et al. (2020), and Singh et al. (2018) documented cases where delayed rehabilitation and prolonged immobilization led to joint stiffness, occlusal derangements, or deviation during function. These issues underscore the importance of patient selection and early physiotherapy in non-surgical protocols.
Comparative studies by Bansal et al. (2021), Kotrashetti et al. (2013), and Prakash et al. (2022) highlighted the heterogeneity in outcome definitions, follow-up durations, and rehabilitation protocols, making pooled analyses challenging. The variability in fixation hardware (e.g., miniplates vs. screws) and surgical access routes (e.g., preauricular vs. retromandibular) adds to the complexity of standardizing ORIF outcomes. Schneider et al. (2008) noted that different surgical routes result in varying levels of nerve involvement and visibility, impacting both recovery and complication rates.
Interestingly, the meta-analytic component of the review (Shobha et al., 2024) showed that CR achieved statistically significant improvements in MIO (SMD = 0.80, p = 0.008), while outcomes in laterotrusion and protrusion favoured CR but lacked statistical significance. These results support the notion that in select cases, conservative management does not compromise functional recovery. However, caution is warranted given the high heterogeneity (I² > 80%) across pooled studies.
Finally, case-specific insights such as those presented by Maeda et al. (2025) and Panneerselvam et al. (2024) suggest that adjunctive technologies-such as low-intensity ultrasound and splint therapy-could further optimize outcomes in CR-treated patients. The findings of Pandey et al. (2024) also support individualized treatment planning, as extracapsular fractures or high condylar displacements may require ORIF to prevent ankyloses or facial asymmetry.
In conclusion, while both CR and ORIF are valid strategies for managing unilateral condylar fractures, the evidence suggests that treatment should be tailored based on patient age, fracture type, displacement degree, and available surgical expertise. As newer minimally invasive and functional rehabilitation techniques evolve, future randomized trials with standardized reporting will be critical to refining clinical protocols and improving patient outcomes.
Conclusion
The systematic review and meta-analysis indicate that both open and closed reduction techniques offer viable management pathways for unilateral mandibular condylar fractures. Closed reduction methods provide superior results in mandibular mobility outcomes such as maximum interincisal opening and are often sufficient for Pediatric or minimally displaced cases. The conservative approach remains the frontline treatment due to its non-invasiveness and low complication profile when appropriately indicated.
Conversely, open reduction with internal fixation shows superiority in anatomical restoration and is especially beneficial for adult patients with moderate to severe displacement or functional compromise. Minimally invasive methods, including endoscopic-assisted ORIF and dynamic elastic CR, are emerging as promising hybrid solutions. Clinical decision-making must remain patient-centered, considering fracture morphology, surgeon experience, and long-term functional needs.
Limitations
This review is limited by heterogeneity in study designs, fracture classification systems, and outcome measurement tools across included studies. The presence of publication bias, high statistical heterogeneity (I² > 80%) in pooled analyses, and variable follow-up durations challenge the consistency of conclusions. Additionally, the lack of standardized rehabilitation protocols and limited representation of multicentre randomized trials may influence external validity.
Future research should focus on well-designed, multicentre randomized controlled trials with standardized outcome reporting, including long-term TMJ function, patient-reported quality-of-life outcomes, and cost-effectiveness analysis of both open and closed interventions.
References
Bansal, A., Yadav, P., Bhutia, O., Roychoudhury, A., & Bhalla, A. S. (2021). Comparison of outcome of open reduction and internal fixation versus closed treatment in pediatric mandible fractures: A retrospective study. Journal of Cranio-Maxillofacial Surgery, 49(3), 196–205.
Bhagol, A., Raj, N., Dahiya, A., Singh, V., Chhikara, D., & Mehta, R. (2024). Evaluation of conventional (static) versus dynamic elastic therapy for closed treatment of unilateral mandibular sub-condylar fractures: A randomized controlled trial. Journal of Maxillofacial and Oral Surgery.
Chrcanovic, B. R. (2012). Open versus closed reduction: Mandibular condylar fractures in children. Oral and Maxillofacial Surgery, 16(3), 257–265.
Didier, T., Morice, A., Laure, B., & Joly, A. (2025). Assessment of pediatric mandibular fracture management in France. Journal of Stomatology, Oral and Maxillofacial Surgery.
Ellis, E. (2013). Open reduction and internal fixation of condylar process fractures. Journal of Oral and Maxillofacial Surgery, 71(11), 1994–2004.
Franke, A., Matschke, J. B., Sembdner, P., Seidler, A., & Cebulla, M. (2025). Long-term outcomes of open treatment of condylar head fractures using cannulated headless bone screws: A retrospective analysis. International Journal of Oral and Maxillofacial Surgery.
Gareikpatii, N. (2021). Study of open versus closed reduction of mandibular condyle fractures. International Surgery Journal, 8(11), 3402–3406.
Huang, C. H., Lee, C. C., Wu, Y. C., Lee, H. C., & Wang, Y. J. (2025). Novel endoscopic‐assisted long plate approach for mandibular condylar fracture reconstruction: A preliminary study. Korean Journal of Medical Science, 41(3).
Jensen, T., Jensen, J., Nørholt, S. E., Dahl, M., Lenk-Hansen, L., & Svensson, P. (2006). Intraoral approach for ORIF of condylar fractures: A long-term follow-up study. Journal of Oral and Maxillofacial Surgery, 64(12), 1771–1779.
Karan, A., Verma, A., Kumar, M., & Bhardwaj, A. (2019). Condylar fractures: Surgical versus conservative management. Annals of Maxillofacial Surgery, 9(1), 15–20.
Khiabani, K. S., Raisian, S., & Khanian, M. M. (2015). Closed vs endoscopic-assisted ORIF in subcondylar fractures. Journal of Maxillofacial and Oral Surgery, 14(2), 363–369.
Kim, S. Y., Ryu, J. Y., Cho, J. Y., & Kim, H. M. (2014). Outcomes of open versus closed treatment in the management of mandibular subcondylar fractures. Journal of the Korean Association of Oral and Maxillofacial Surgeons, 40(6), 297–300.
Kokemueller, H., Konstantinovic, V. S., Barth, E. L., Essig, H., & Tavassol, F. (2012). Endoscope-assisted transoral reduction and internal fixation vs closed treatment: A prospective study. Journal of Oral and Maxillofacial Surgery, 70(2), 384–395.
Kotrashetti, S. M., Lingaraj, J. B., & Khurana, V. (2013). Comparison of closed vs open treatment in subcondylar fracture. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, 115(4), e7–e11.
Landes, C. A., & Lipphardt, R. (2005). Open reduction and internal fixation of displaced condylar head fractures. International Journal of Oral and Maxillofacial Surgery, 34(8), 859–870.
Maeda, K., Yamamoto, S., & Taniike, N. (2025). Long-term stability after bilateral condylar fracture with symphyseal involvement: Case series. Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology.
Pandey, S., Simre, S. S., Chaulagain, R. S., Vyas, A., & Upadhyaya, R. (2024). Open reduction internal fixation versus closed reduction for the management of mandibular intra-capsular fractures in adult patients: A systematic review and meta-analysis. Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology.
Panneerselvam, E., Yalagala, V. S., Sinha, V., Sharma, K., & Ramesh, C. (2024). Non-invasive management of mandibular condyle fracture with ramus shortening using low intensity pulsed ultrasound and hypomochlion splint. Journal of Maxillofacial and Oral Surgery.
Prakash, R. Sr., Nair, R. K., & Arun, A. (2022). ORIF versus MMF of condylar fractures of the mandible: A prospective study. Cureus, 14(1), e21186.
Rashid, A., Mumtaz, M., Asif, J., & Azeem, M. (2020). Effect of treatment on occlusal relationship in mandibular condyle fractures. Pakistan Oral & Dental Journal, 34(1).
Schneider, M., Lauer, G., Eckelt, U., & Runte, C. (2008). Open reduction vs closed treatment of mandibular condylar process fractures. Journal of Oral and Maxillofacial Surgery, 66(12), 2537–2544.
Shobha, E. S., Nainoor, N., Prashanth, N. T., Rangan, V., Malick, R., & Shetty, S. (2024). Comparative evaluation of open reduction with internal fixation against closed reduction methods for condylar fracture management: A systematic review and meta-analysis. Journal of Maxillofacial and Oral Surgery, 23, 475–487.
Singh, V., Srivastava, A., Jaiswal, R., & Kapoor, A. (2018). Open vs closed management in displaced subcondylar fractures. Craniomaxillofacial Trauma & Reconstruction, 11(3), 205–210.
Stypulkowski, R. P., Santos, A. G., Paula Silva, E., Costa Moraes, C. A., & Rosa, E. L. (2019). Unilateral mandibular condylar process fractures: A retrospective clinical comparison of open versus closed treatment. Oral and Maxillofacial Surgery, 23(1), 209–214.
Throckmorton, G. S., & Ellis, E. (2000). Recovery of mandibular motion after closed and open treatment of unilateral mandibular condylar process fractures. International Journal of Oral and Maxillofacial Surgery, 29(6), 421–427.
Zhou, H., Zhang, J., & Luo, Y. (2018). Comparative analysis of condylar neck fractures treated with open versus closed approaches. British Journal of Oral and Maxillofacial Surgery, 56(1), 35–39.