Research Article - (2023) Volume 18, Issue 6
Correlation Between Cognitive Pain Perception And Functional Performance Level In Patients With Chronic Nonspecific Low
Ehab A. Abdallah1*, Taher Salah El-Din Taha2,3, Sobhy M. Aly4,5, Hamada S. Abulkhair6,7 and Mahmoud D. Abdelhaleem8*Correspondence: Ehab A. Abdallah, Department of Orthopedic Physical Therapy, Faculty of Physical Therapy, Horus University-Egypt, New Damietta, Egypt, Email:
2Fellow of Physical Therapy, Sohag Teaching Hospital, Sohag, Egypt
3Department of Pediatric Physical Therapy, Mayo University, Egypt
4Department of Biomechanics, Faculty of Physical Therapy, Cairo University, Giza, Egypt
5Department of Medical Rehabilitation Sciences, Najran University, KSA
6Department of Pharmaceutical Organic Chemistry, Faculty of Pharmacy, Al-Azhar University, Nasr City, Cairo, Egypt
7Department of Pharmaceutical Organic Chemistry, Faculty of Pharmacy, Horus University-Egypt, International Coastal Road, New Damietta, Egypt
8Department of Orthopedic Physical Therapy, Faculty of Physical Therapy, Cairo University, Giza, Egypt
Received: 15-Dec-2023 Published: 20-Dec-2023
Abstract
Background: However, the prevalence of chronic low back pain is high; the relation between pain perception and poor functional performance among these patients is still unclear. Therefore, this study aimed to investigate the relation between cognitive awareness and functional performance in patients with chronic low back pain.
Methods: 120 patients were enrolled in the study as one group. All patients were diagnosed with chronic nonspecific low back pain (CNLBP) and their mean Age was 32.43 ± 5.77 years. The Visual Analog Scale was used to assess pain intensity, fair avoidance and believe questionnaire was used to assess the social and behavioral aspects of the subject and Oswestry disability index was used to assess the functional performance level.
Statistics: Pearson correlation coefficient was carried-out to examine the correlation among Oswestry disability index, VAS, fair avoidance and believe questionnaire/work, as well as fair avoidance and believe questionnaire/ life. The variables with a significant correlation with Oswestry disability index findings were identified using multiple linear regressions. A significance level of p < 0.05 was established for statistical testing.
Results: Statistical analysis revealed that the Oswestry disability index was strongly correlated with FABQW (r = 0.915, p = 0.001), FABQPA (r = 0.866, p = 0.001), and VAS (r = 0.891, p = 0.001). The VAS had a strong positive correlation with FABQW (r = 0.951, p = 0.001) and with FABQPA (r = 0.915, p = 0.001). Conclusion: Our study reflects the probable impact of CNLBP as an underlying cause of altered cognitive behavior and consequently reduced functional performance.
Keywords
Back pain, Pain perception, Fair avoidance and believe questionnaire, Visual analog scale, Oswestry disability index
Introduction
Pain is a physiological process that results from a disturbance that activates a response all over the body and alarms about serious issues that the body faces and could prevent further damage (Arntz & Claassens, 2004; Fink, 2000; Suresh et al., 2023). The literature survey showed that it could be a protective mechanism that prevents the patients from excessively using painful regions and assists in physiological homeostasis of the tissue (Gatchel et al., 2007; Arntz & Claassens, 2004; Asai et al., 2002). Acute pain is described as a sharp consistent pain that almost lasts for less than fourteen days (Fink, 2000). Chronic pain is described as pain that consumes longer period and characterized with lower intensity than acute pain and could last up to three months (Johns Hopkins University, 2023; Mills et al., 2019). Common causes of pain are acute illness, injury, dental work, childbirth, cuts, infections and surgical operations (Neil & Macrae, 2009). The chronicity of the pain does affect the patient negatively as it becomes a belief for him that the pain will stay for good. Persisting pain that continues longer than the usual healing time represents a barrier to one’s health (Hickey, Joanne V.; Strayer, 2019; Vardeh et al., 2016; Reid et al., 2015). Longstanding pain is difficult to manage where more than half of the patients are expected to encounter pain longer than a year of treatment (Butchart et al., 2009). In the same vein, clinical studies concluded that psychological disturbance and moderate to severe depression were encountered by 85% of patients suffering from chronic pain (Hickey, Joanne V.; Strayer, 2019; Sheng et al., 2017). The human body can release certain chemical substances in response to these pain sources, and accordingly, the pain subsides with time, its intensity becomes less sharp, and patients feel better (Saracoglu et al., 2021; Gatchel et al., 2007).
The literature supports the fact that chronic pain induces structural changes in the subject's brain which indeed make the management of such an issue hard to overcome (Crofford, 2015). Recurrent pain has the potential to cause a disorder of maladaptive behavior and cognition, which in turn can reduce productivity in daily tasks, exacerbate psychological stress, and potentially make the pain last longer (vicious circle) (Hnatešen et al., 2022; Asmundson et al., 2012). Patients with chronic pain complain of psychological disorders (Crofford, 2015). Epidemiologic research revealed strong evidence for a strong association among chronic pain and psychological dysfunction but doesn’t examine whether chronic pain lead to perception dysfunction or vice versa (Fairbank & Pynsent, 2000; Mills et al., 2019; van Hecke et al., 2013).
Indeed, any onset of the pain problem could be associated with social and emotional malfunctions. Numerous individuals with chronic pain, particularly those with disabilities who visit pain clinics, have a history of depression that occurred years before their pain condition, according to several studies (Lall & Restrepo, 2017). Fatigue, sleep disturbances, and loss of appetite are somatic symptoms that are often accompanying long-lasting pain (Orzechowska et al., 2021). The emotional, motivational, cognitive, as well as psychosocial components of chronic pain are more pronounced than the pain itself that is linked to pain itself. (Bushnell et al., 2013; Simons et al., 2014). As a symptom, the pain could result from structural injury or inflammation at a body part and the chronicity of the pain in fact has impact of the subject perception and cognitive orientation of the problem itself (Linton & Shaw, 2011).
That is why the authors have decided to conduct the current study. In this study, the authors aimed to investigate the relation between functional performance of the patients with chronic consistent pain and cognitive perception and behavioral changes in patients with chronic low back pain. As part of our contribution to the scientific research (Abdallah et al., 2023; Abdelhaleem et al., 2022, 2023; Abulkhair et al., 2021; El-Adl et al., 2021; Ihmaid et al., 2017; Kutkat et al., 2022), the current study aimed to assess pain intensity of chronic non-specific low back pain (CNLBP) patients and how they act physically and psychologically in response to such a trauma. Answers to this question would be a critical tread toward solving the maze of chronicity of low back pain and breaking the vicious circle that includes pain led to malfunctions that lead to psychological disorders.
Materials and method
Study Design This study is conducted using a cross-sectional design and adheres to the principles outlined in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) declaration. Furthermore, it complies with the standards specified in the Declaration of Helsinki.
Settings
The research study aims to recruit patients with low back pain lasting at least three months. The study duration is scheduled from 1st of August to 30th November 2023. Patients will be recruited at the Sohag Educational Hospital from 20/7/2023 to 30/9/2023. The research plan has received approval from the research ethical committee of the faculty of physical therapy at Cairo University, with the reference number P.T.REC/012/004702, granted on July 18, 2023.
Sample recruitment
The study selected 120 patients diagnosed with CNLBP from a private outpatient clinic located in Al-Giza, Sohag and Quesna. The clinic specifically mentioned is the Al-Rawan private physiotherapy center in Quesna city, which is situated in the Menofia governate of Egypt.
Inclusion criteria
The inclusion criteria include patients between 21 and 45 years with low back pain lasting over three months, attending physiotherapy out-patient centers. The exclusion criteria consist of individuals with cauda equina syndrome, tumors, infection, previous surgery of the spine, pregnancy, pain with menstruation, and psychological illness.
Assessment procedure
Three physical therapists, one male and two female, conducted personal interviews to gather the data that was subsequently analyzed. Data was collected using a standardized questionnaire presented by an interviewer in person. Before participation, all individuals were required to sign an informed consent document.
Pain intensity using VAS (Visual Analog Scale)
It is used to evaluate low back pain (LBP) intensity (Haefeli & Elfering, 2006; Subramanian & Venkatesan, 2022). Study patients indicate their pain intensity by selecting a single number on a scale ranging from zero (no pain) to ten (maximum pain).
FABQ (Fear Avoidance Beliefs Questionnaire)
It is a patient-reported questionnaire used to assess how an individual's fear avoidance beliefs regarding physical activity as well as work contribute to their LBP and resulting disability (Waddell et al., 1993). The FABQ assesses fear of pain in addition to avoidance of physical activity, covering various areas such as daily activities, behavior, health, mental well-being, and much more. There are sixteen items in the questionnaire, and patients are asked to rate their level of fear avoidance using a 7-point Likert scale. It consists of two subscales: a seven-item work subscale (FABQw) and a four-item physical activity subscale (FABQPA). Scoring method for fear-avoidance beliefs concerning work items 6, 7, 9, 10, 11, 12, 15, and for fear-avoidance beliefs concerning physical activity items 2, 3, 4, 5 are counted. (Arabic and English version of FABQ supplementary 1).
Oswestry low back disability questionnaire:
It is a scale of ten questions assessing functional performance level (Fairbank & Pynsent, 2000). The questions cover various areas such as pain severity, individual care, lifting, walking, sitting, standing, sleeping, social life, traveling, as well as employment/homemaking. The scoring of each question is based on a scale of 0 to 5, with a greater score indicating larger disability. The total score is used to determine the disability level, ranging from no disability to complete disability. (Arabic and English version of Oswestry low-back disability questionnaire, supplementary 2)
Statistical analysis
The demographic and clinical data of the patients were presented using descriptive statistics. According to Mishra et al. (2019), the Shapiro-Wilk test was used to ensure that the data was normal. An investigation of the correlation among ODI, VAS, FABQW, and FABQPA was carried out using the Pearson correlation coefficient. The factors significantly associated with ODI outcomes were identified using multiple linear regression. A p-value less than 0.05 was established as the threshold for statistical significance. Statistical analysis was carried out using the Windows version 25 of the statistical software for the social sciences (SPSS).
Results
Subject characteristics
One hundred and twenty patients with LBP took part in this study. Their mean ± SD age was 32.43 ± 5.77 years with a minimum of 21 years and maximum of 45 years. Th mean ± SD duration of pain was 6.25 ± 2.77. Female patients represented 59.2% while male patients were 40.8% (Tables 1 and 2).
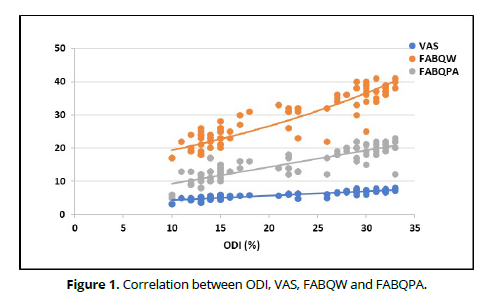
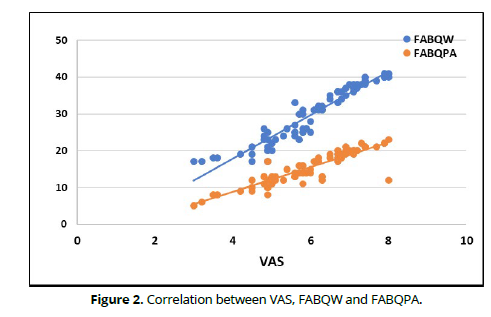
SD = Standard deviation ODI, VAS, FABQW and FABQPA in patients with LBP: The ODI of patients with LBP ranged from 10 to 33% with mean ± SD 22.09 ± 7.81. The mean ± SD of VAS, FABQW and FABQPA were 5.96 ± 1.22, 29.48 ± 7.61 and 15.42 ± 4.52, respectively. (Table 3). Correlation between ODI, VAS, FABQW and FABQPA in patients with LBP: The correlations of ODI were strong positive correlation with FABQW (r = 0.915, p = 0.001), FABQPA (r = 0.866, p = 0.001) and with VAS (r = 0.891, p = 0.001). The correlations of VAS were strong positive correlation with FABQW (r = 0.951, p = 0.001) and with FABQPA (r = 0.915, p = 0.001) (Table 4, Figures 1& 2).
| Descriptor | Mean ±SD | Minimum | Maximum |
|---|---|---|---|
| Age (years) | 32.43 ± 5.77 | 21 | 45 |
| Weight (kg) | 72.32 ± 11.57 | 53 | 102 |
| Height (cm) | 168.22 ± 7.03 | 149 | 191 |
| BMI (kg/m²) | 25.49 ± 3.12 | 20.07 | 40.54 |
| Duration of LBP (months) | 6.25 ± 2.77 | 1 | 14 |
SD = Standard deviation
Descriptor |
Number | Percentage | |
|---|---|---|---|
| Sex | Females | 71 | 59.2% |
| Males | 49 | 40.8% | |
| ODI | Mild | 32 | 26.7% |
| Moderate | 35 | 29.2% | |
| Sever | 53 | 44.2% |
| Descriptor | Mean ± SD | Minimum | Maximum |
|---|---|---|---|
| ODI | 22.09 ± 7.81 | 10 | 33 |
| VAS | 5.96 ± 1.22 | 3 | 8 |
| FABQW | 29.48 ± 7.61 | 17 | 41 |
| FABQPA | 15.42 ± 4.52 | 5 | 23 |
SD = Standard deviation
Prediction of ODI score
Multiple linear regression analysis showed that the total model explained 84% of the variance of ODI score. FABQW was a significant predictor of ODI score (p < 001) while VAS and FABQPA were not significant predictors of ODI (Table 5).
Model |
B | t | p- value | 95% CI | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| VAS | 1.07 | 1.33 | 0.18 | -0.52 | 2.67 |
| FABQW | 0.66 | 4.97 | 0.001 | 0.40 | 0.92 |
| FABQPA | 0.21 | 1.21 | 0.23 | -0.13 | 0.55 |
B: Regression coefficient; value: p-value, probability value.
Discussion
The biopsychosocial model of CNSLBP reveals a valuable guideline to understand how chronic low back pain impacts biological, psychological, and social aspects of these patients. The model is built on a holistic approach sight that any disease has different dimensions and that how an individual who is experiencing chronicity in their pain interacts biologically, psychologically, and socially to such pain (Meints & Edwards, 2018).
The literature started, in 1970, to introduce the biopsychosocial model, and it was a challenge for the well-developed biomedical model of disease. The latter represents a viewpoint that holds that diseases are caused by apparent biological processes and that these processes alone should be considered while managing diseases. Thus, according to Lall and Restrepo (2017), medical professionals and researchers who adhere to the biomedical model would examine lumbar spinal abnormalities, biochemical defects, and neurophysiological distortions as potential causes of LBP. In contrast, those who follow the biopsychosocial model would consider a wide range of factors, including social disorders such as level of education and employment as well as psychological conditions like anxiety and depression. The biological model offers a strong pathophysiological foundation for disease research, but its critics continually point out that it can't account for individual differences in how individuals experience and respond to disease. Similarly, lumbar spine imaging studies often reveal comparable findings in patients, but their clinical presentations can vary greatly; for example, some patients may show no symptoms at all, while others may report moderate pain, and yet others may describe severe pain (Andersen et al., 2019). While outlining the bio psychosocial model's proper application to LBP, Waddell (1987) made a distinction between CLBP and (low back dysfunction) LBD. According to his description, LBP is a benign, self-limiting condition that manifests itself in a variety of ways depending on the specific abnormalities that caused it, such as via physical trauma or mechanical overloading. on the other hand, he considered LBD as a disorder defined by excessively tormenting behaviors that do not correspond to any obvious abnormalities, and it is the product of a complicated relationship between biological, psychological, as well as social elements.
The present study was carried-out to investigate the relationship among the social aspect and pain perception of patients who suffer from CNLBP and the functional performance of these patients. The authors aimed to assess how much the impact between the biopsychosocial status and how patients with CNLBP practice their life and work. On the same vein, the present study was performed to examine the correlation among the pain severity of patients with CNLBP and if their a relation between this intensity, functional productivity and social perspectives of these patients The findings of the present study prove that there is a strong relation between how the patients with CNSLBP feel and percept the chronic pain and how they practice their daily life routine at home with family and at work. Statistical analysis revealed that the correlations of ODI were strong positive correlation with FABQW (r = 0.915, p = 0.001), FABQPA (r = 0.866, p = 0.001) and with VAS (r = 0.891, p = 0.001). and the correlations of VAS were strong positive correlation with FABQW (r = 0.951, p = 0.001) and with FABQPA (r = 0.915, p = 0.001). (Table 4, Figures 1 and 2).
The findings of the present study link between the two models, the biomedical model and the bio psychosocial model as the results revealed that both functional and social aspects of patient are affected. It comes with the philosophy that the subject is a one unit who his perception got affected by any disorders and any disorder management is leaded by how much the patient is well oriented and psychological stable. Results presented here agree with the review performed by Lall and Restrepo 2017. The latter concluded that there is a significant association among biological, psychological, social aspects and pain severity, functional disability, and return to work. The biopsychosocial model (psychological along with social factors) could impact patient outcomes.
On these terms, several studies agree with the current one. These studies concluded that most chronic pain patients suffer from depression (Romano & Turner, 1985 (Romano & Turner, 1985); Banks & Kerns, 1996 (Banks & Kerns, 1996); Dersh et al., 2006 (Dersh et al., 2006);). Although there is strong evidence among depression and chronic pain, the studies do not address the question of which occurs first: depression causing chronic pain or chronic pain causing depression. According to Brown (1990), who supported the theory that pain produces depression, depressed episodes frequently started after the painful problem had already begun. A number of research have shown that many people who suffer from chronic pain actually had a history of depression that was years before their pain condition ("Chronic Pain: Lifetime Psychiatric Diagnoses and Family History," 1985), even if most studies seem to support this opinion.
Mood and chronic low back pain factors were analyzed by Fracaro and his colleges in 2013, they concluded that patients who had depression, anger, fatigue, tension and mental confusion suffer from physical dysfunctions and walk in slower cadence and unsteady patterns (Fracaro et al., 2013). On these terms, Sardá Jr., Kupek and Cruz revealed that patients with CLBP have poorer mental health in compare with normal patients, Also, they stated that symptoms related to LBP and to lumbo-sacral dysfunctions have a strong relationship with patients’ psychological changes (Sardá Junior et al., 2009). In the same vein, the necessity of investigating the impact of biopsychosocial factors on assessing CNLBP may provide support for the biopsychosocial model of CLBP. Also, studies investigating the associations among biopsychosocial factors and CLBP may show additional support for the biopsychosocial model of LBP by providing evidence for the hypothesized relationship among biological, psychological, and social factors and LBP.
Conclusion
While dealing with patients who suffer from chronic low back pain, clinicians are needed to examine their pain perception status and cognitive awareness of the changes that occurred by chronic pain. Understanding the relation will guide both clinician and patient to get rid of such a challenging problem. Although previous reports have concluded that most chronic pain patients suffer from altered cognitive behavior, none of them has clarified which one comes first, whether chronic pain causes altered cognitive behavior or altered cognitive behavior causes chronic pain. Our study reflects the probable impact of CNLBP as an underlying cause of altered cognitive behavior and consequently reduced functional performance.
Limitations
1. Patients with other kinds of low back pain were not included in the study, thus the implications should not apply to them. 2. The duration of illness of a CNLBP patient's disease varies greatly.
Implications for physiotherapy practice
When treating low back pain, physiotherapists should consider both the biological and biopsychosocial aspects of pain.
Recommendation for future research
Future research on the management of chronic nonspecific low back pain should compare cognitive training with traditional methods, considering this study's findings.
References
Abdallah, E., Neamat Allah, N. H., Abdelhay, M. I., Mousa, N., Abdelhaleem, M. D., Aly, S., & Nadier, A. (2023). Effectiveness of Eccentric Strengthening Exercises on Pain and Functional Abilities in Patients with Knee Osteoarthrosis: A Randomized Clinical Trial. Egyptian Journal of Physical Therapy, 13(1), 28–34. https://doi.org/10.21608/ejpt.2022.145128.1089
Abdelaty, E. M., Shendy, S., Lotfy, O., & Hassan, K. A. (2023). The difference in multifidus muscle morphology and motor control in non‐specific low back pain with clinical lumbar instability and healthy subjects: A case‐control study. Physiotherapy Research International. https://doi.org/10.1002/pri.2047
Abdelhaleem, M. D., Abdallah, E. A., Neamat Allah, N. H., Zaitoon, Z. M., Zahran, S. S., & Abdelhay, M. I. (2022). Effect of simultaneous application of positional release technique and Maitland mobilization technique on sciatica: a randomized controlled trial. Bulletin of Faculty of Physical Therapy, 27(1), 29. https://doi.org/10.1186/s43161-022-00089-5
Abdelhaleem, M. D., Abdelhay, M. I., Aly, S. M., Abdallah, E. A., & Neamat Allah, N. H. (2023). Effects of 6 weeks of ankle stability exercises on pain, functional abilities, and flexibility in patients with chronic non-specific low back pain: a randomized controlled trial. Bulletin of Faculty of Physical Therapy, 28(1), 14. https://doi.org/10.1186/s43161-023-00126-x
Abulkhair, H. S., Elmeligie, S., Ghiaty, A., El-Morsy, A., Bayoumi, A. H., Ahmed, H. E. A., El-Adl, K., Zayed, M. F., Hassan, M. H., Akl, E. N., & El-Zoghbi, M. S. (2021). In vivo- and in silico-driven identification of novel synthetic quinoxalines as anticonvulsants and AMPA inhibitors. Archiv Der Pharmazie, 354(5), 2000449. https://doi.org/10.1002/ardp.202000449
Andersen, F., Anjum, R. L., & Rocca, E. (2019). Philosophical bias is the one bias that science cannot avoid. ELife, 8. https://doi.org/10.7554/eLife.44929
Arntz, A., & Claassens, L. (2004). The meaning of pain influences its experienced intensity. Pain, 109(1), 20–25. https://doi.org/10.1016/j.pain.2003.12.030
Asai, T., Kusudo, K., Ikeda, H., & Murase, K. (2002). Intrinsic optical signals in the dorsal horn of rat spinal cord slices elicited by brief repetitive stimulation. European Journal of Neuroscience, 15(11), 1737–1746. https://doi.org/10.1046/j.1460-9568.2002.02006.x
Asmundson, G. J., Noel, M., Petter, M., & Parkerson, H. A. (2012). Pediatric Fear-Avoidance Model of Chronic Pain: Foundation, Application and Future Directions. Pain Research and Management, 17(6), 397–405. https://doi.org/10.1155/2012/908061
Banks, S. M., & Kerns, R. D. (1996). Explaining high rates of depression in chronic pain: A diathesis-stress framework. Psychological Bulletin, 119(1), 95–110. https://doi.org/10.1037/0033-2909.119.1.95
Brown, G. K. (1990). A causal analysis of chronic pain and depression. Journal of Abnormal Psychology, 99(2), 127–137. https://doi.org/10.1037/0021-843X.99.2.127
Bushnell, M. C., Čeko, M., & Low, L. A. (2013). Cognitive and emotional control of pain and its disruption in chronic pain. Nature Reviews Neuroscience, 14(7), 502–511. https://doi.org/10.1038/nrn3516
Butchart, A., Kerr, E. A., Heisler, M., Piette, J. D., & Krein, S. L. (2009). Experience and Management of Chronic Pain Among Patients With Other Complex Chronic Conditions. The Clinical Journal of Pain, 25(4), 293–298. https://doi.org/10.1097/AJP.0b013e31818bf574
Chronic pain: lifetime psychiatric diagnoses and family history. (1985). American Journal of Psychiatry, 142(10), 1156–1160. https://doi.org/10.1176/ajp.142.10.1156
Crofford, L. J. (2015). Chronic Pain: Where the Body Meets the Brain. Transactions of the American Clinical and Climatological Association, 126, 167–183. http://www.ncbi.nlm.nih.gov/pubmed/26330672
Dersh, J., Gatchel, R. J., Mayer, T., Polatin, P., & Temple, O. R. (2006). Prevalence of Psychiatric Disorders in Patients With Chronic Disabling Occupational Spinal Disorders. Spine, 31(10), 1156–1162. https://doi.org/10.1097/01.brs.0000216441.83135.6f
El-Adl, K., Sakr, H., El-Hddad, S. S. A., El-Helby, A. G. A., Nasser, M., & Abulkhair, H. S. (2021). Design, synthesis, docking, ADMET profile, and anticancer evaluations of novel thiazolidine-2,4-dione derivatives as VEGFR-2 inhibitors. Archiv Der Pharmazie, 354(7), 2000491. https://doi.org/10.1002/ardp.202000491
Fairbank, J. C. T., & Pynsent, P. B. (2000). The Oswestry Disability Index. Spine, 25(22), 2940–2953. https://doi.org/10.1097/00007632-200011150-00017
Fink, R. (2000). Pain Assessment: The Cornerstone to Optimal Pain Management. Baylor University Medical Center Proceedings, 13(3), 236–239. https://doi.org/10.1080/08998280.2000.11927681
Fracaro, G. de A., Bertor, W. R. R., Silva, L. I. da, Brandl, L., Zanini, G. M., Zilio, M., Agnol, E. D., Rocha, B. P., & Carvalho, A. R. de. (2013). Comparação entre variáveis psicossociais e de desempenho funcional em um grupo de pacientes com lombalgia crônica. Revista Dor, 14(2), 119–123. https://doi.org/10.1590/S1806-00132013000200009
Ganesh, G. S., Chhabra, D., & Mrityunjay, K. (2015). Efficacy of the Star Excursion Balance Test in Detecting Reach Deficits in Subjects with Chronic Low Back Pain. Physiotherapy Research International, 20(1), 9–15. https://doi.org/10.1002/pri.1589
Gatchel, R. J., Peng, Y. B., Peters, M. L., Fuchs, P. N., & Turk, D. C. (2007). The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychological Bulletin, 133(4), 581–624. https://doi.org/10.1037/0033-2909.133.4.581
Haefeli, M., & Elfering, A. (2006). Pain assessment. European Spine Journal, 15(S1), S17–S24. https://doi.org/10.1007/s00586-005-1044-x
Hickey, Joanne V.; Strayer, A. L. (2019). Clinical Practice of Neurological and Neurosurgical Nursing (8th ed.). Lippincott Williams & Wilkins (LWW). https://www.wolterskluwer.com/en/solutions/ovid/clinical-practice-of-neurological-and-neurosurgical-nursing-the-1773
Hnatešen, D., Pavić, R., Radoš, I., Dimitrijević, I., Budrovac, D., Čebohin, M., & Gusar, I. (2022). Quality of Life and Mental Distress in Patients with Chronic Low Back Pain: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(17), 10657. https://doi.org/10.3390/ijerph191710657
Ihmaid, S., Ahmed, H. E. A., Al-Sheikh Ali, A., Sherif, Y. E., Tarazi, H. M., Riyadh, S. M., Zayed, M. F., Abulkhair, H. S., & Rateb, H. S. (2017). Rational design, synthesis, pharmacophore modeling, and docking studies for identification of novel potent DNA-PK inhibitors. Bioorganic Chemistry, 72, 234–247. https://doi.org/10.1016/j.bioorg.2017.04.014
Johns Hopkins University. (2023). Chronic Pain. https://www.hopkinsmedicine.org/health/conditions-and-diseases/chronic-pain#:~:text=Chronic pain is long standing,physical activity%2C or enjoy life.
Kutkat, O., Moatasim, Y., Al‐Karmalawy, A. A., Abulkhair, H. S., Gomaa, M. R., El-Taweel, A. N., Abo Shama, N. M., GabAllah, M., Mahmoud, D. B., Kayali, G., Ali, M. A., Kandeil, A., & Mostafa, A. (2022). Robust antiviral activity of commonly prescribed antidepressants against emerging coronaviruses: in vitro and in silico drug repurposing studies. Scientific Reports, 12(1), 12920. https://doi.org/10.1038/s41598-022-17082-6
Lall, M. P., & Restrepo, E. (2017). The Biopsychosocial Model of Low Back Pain and Patient-Centered Outcomes Following Lumbar Fusion. Orthopaedic Nursing, 36(3), 213–221. https://doi.org/10.1097/NOR.0000000000000350
Linton, S. J., & Shaw, W. S. (2011). Impact of Psychological Factors in the Experience of Pain. Physical Therapy, 91(5), 700–711. https://doi.org/10.2522/ptj.20100330
Meints, S. M., & Edwards, R. R. (2018). Evaluating psychosocial contributions to chronic pain outcomes. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 87, 168–182. https://doi.org/10.1016/j.pnpbp.2018.01.017
Mills, S. E. E., Nicolson, K. P., & Smith, B. H. (2019). Chronic pain: a review of its epidemiology and associated factors in population-based studies. British Journal of Anaesthesia, 123(2), e273–e283. https://doi.org/10.1016/j.bja.2019.03.023
Mishra, P., Pandey, C., Singh, U., Gupta, A., Sahu, C., & Keshri, A. (2019). Descriptive statistics and normality tests for statistical data. Annals of Cardiac Anaesthesia, 22(1), 67. https://doi.org/10.4103/aca.ACA_157_18
Neil, M. J., & Macrae, W. A. (2009). Post Surgical Pain- The Transition from Acute to Chronic Pain. Reviews in Pain, 3(2), 6–9. https://doi.org/10.1177/204946370900300203
Orzechowska, A., Maruszewska, P., & Gałecki, P. (2021). Cognitive Behavioral Therapy of Patients with Somatic Symptoms—Diagnostic and Therapeutic Difficulties. Journal of Clinical Medicine, 10(14), 3159. https://doi.org/10.3390/jcm10143159
Reid, M. C., Eccleston, C., & Pillemer, K. (2015). Management of chronic pain in older adults. BMJ, 350(feb13 2), h532–h532. https://doi.org/10.1136/bmj.h532
Romano, J. M., & Turner, J. A. (1985). Chronic pain and depression: does the evidence support a relationship? Psychological Bulletin, 97(1), 18–34. http://www.ncbi.nlm.nih.gov/pubmed/3983297
Saracoglu, I., Aksoy, C. C., Afsar, E., & Arik, M. I. (2021). Does pain neuroscience education improve pain knowledge, beliefs and attitudes in undergraduate physiotherapy students? Physiotherapy Research International, 26(2). https://doi.org/10.1002/pri.1898
Sardá Junior, J. J., Kupek, E., Cruz, R. M., Bartilotti, C., & Cherem, A. J. (2009). Preditores de retorno ao trabalho em uma população de trabalhadores atendidos em um programa de reabilitação profissional. Acta Fisiátrica, 16(2), 81–86. https://doi.org/10.11606/issn.2317-0190.v16i2a103176
Sheng, J., Liu, S., Wang, Y., Cui, R., & Zhang, X. (2017). The Link between Depression and Chronic Pain: Neural Mechanisms in the Brain. Neural Plasticity, 2017, 1–10. https://doi.org/10.1155/2017/9724371
Simons, L. E., Elman, I., & Borsook, D. (2014). Psychological processing in chronic pain: A neural systems approach. Neuroscience & Biobehavioral Reviews, 39, 61–78. https://doi.org/10.1016/j.neubiorev.2013.12.006
Subramanian, M., & Venkatesan, P. (2022). The predictors for altered central pain modulation in individuals with nonspecific chronic low back pain: A systematic review. Pain Practice, 22(2), 276–284. https://doi.org/10.1111/papr.13081
Suresh, V., Venkatesan, P., & Babu, K. (2023). Effect of proprioceptive neuromuscular facilitation and cranio‐cervical flexor training on pain and function in chronic mechanical neck pain: A randomized clinical trial. Physiotherapy Research International. https://doi.org/10.1002/pri.2058
van Hecke, O., Torrance, N., & Smith, B. H. (2013). Chronic pain epidemiology – where do lifestyle factors fit in? British Journal of Pain, 7(4), 209–217. https://doi.org/10.1177/2049463713493264
Vardeh, D., Mannion, R. J., & Woolf, C. J. (2016). Toward a Mechanism-Based Approach to Pain Diagnosis. The Journal of Pain, 17(9), T50–T69. https://doi.org/10.1016/j.jpain.2016.03.001
WADDELL, G. (1987). 1987 Volvo Award in Clinical Sciences: A New Clinical Model for the Treatment of Low-Back Pain. Spine, 12(7), 632–644. https://doi.org/10.1097/00007632-198709000-00002
Waddell, G., Newton, M., Henderson, I., Somerville, D., & Main, C. J. (1993). A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoisdance beliefs in chronic low back pain and disability. Pain, 52(2), 157–168. https://doi.org/10.1016/0304-3959(93)90127-B