Research Article - (2024) Volume 19, Issue 1
*Correspondence: Shrouk Abd Elmohsen Elnhrawy, Physiotherapist at Kafr Jaafar Medical Center, Gharbia Governorate, Egypt, Email:
2Assistant Professor, Department of Physical Therapy for Pediatrics, Faculty of Physical Therapy, Kafrelsheikh University, Egypt
3Consultant of Orthopaedic Surgery, Damanhour Teaching Hospital, Elbehaira, Egypt
4Lecturer, Department of Physical Therapy for Pediatrics, Faculty of Physical Therapy, Kafrelsheikh University, Egypt
Received: 15-Feb-2024 Published: 21-Feb-2024
Abstract
Abstract Background: Polyarticular juvenile idiopathic arthritis is represented with chronic pain and inflammation, and extra-articular manifestations with elevated comorbidities resulted in massive socio-economic impacts. Both pulsed electromagnetic fields, and low-level laser therapies are non-invasive therapeutic approaches have anabolic benefits those not fully explored so far.
Purpose: To compare between pulsed magnetic field versus low level laser therapy in management of polyarticular juvenile idiopathic arthritis.
Material & Methods: A single prospective clinical, randomized control trial. It involved forty children with polyarticular juvenile idiopathic arthritis, their age range was 8-16 years old, and they were randomly assigned into two equal groups Group (A): received pulsed electromagnetic field, in addition to standard physical therapy program. Group (B): received low intensity laser therapy, in addition to standard physical therapy program. All children were trained one hour per day, three times a week, as well pretreatment and at two months post treatment values were measured and analyzed.
Results: No significant differences at baseline evaluation. Significant increase in group A in terms of knee flexion by 23.84% than group B by 13.92%, and for extension by 16.97% than for group B by 13.72%, also significant decrease in group A in terms of knee circumference at and above patella, also Arabic version of Childhood Health Assessment Questionnaire values by 78.9%, 11.83% and 11.53%, while group B were 66.17%, 5.66%, and 6.09%, respectively.
Conclusions: It can be concluded that pulsed magnetic field produces better therapeutic improvement in compare to low-level laser therapy in management of children aged 8-16 years old with polyarticular juvenile idiopathic arthritis.
Keywords
Polyarticular juvenile idiopathic arthritis, Digital goniometer, Lowlevel laser therapy, Pulsed magnetic field therapy.
Introduction
Polyarticular juvenile idiopathic arthritis (PJIA) is a medical broad term addresses a clinical heterogeneous chronic polyarthritis disorder with unknown causes that manifested with persistent joint inflammation, extraarticular manifestations with elevated comorbidity risks for whom less than 16 years old (1). Worldwide estimated PJIA prevalence is around three million children, with lowest incidence was 3.43 per 100.000 in Egypt (2,3). Up to date, no definite diagnostic criteria with variety of involved joints affection, disease activity, and associated clinical signs (4).
Recent update of International League of Associations of Rheumatology (ILAR) has proposed classification criteria for PJIA into seven subdivisions those have varying clinical features, and are globally used for whom disease onset prior to 16 years old for at least one joint affection persisting >6 weeks (5,6).
Children with PJIA have multiple clinical manifestations that obvious restrict their daily living due to persistent joint pain, and swelling, morning stiffness, limited locomotors and possible ocular infirmities those cause short-term, and long-term (7,8).
Despite novel biological therapeutic approaches, unless many PJIA children may still have a progressive clinical course. For optimal PJIA management its vital to have supportive measures i.e., adequate nutritional support including Ca2+, vitamin D …etc. those are multi-faceted approach to preserve mobility, musculoskeletal strength and functioning, also reduce remission, and possible systemic comorbidities (9-10).
Pulsed electromagnetic field (PEMF) therapy is a FDA-approved non-invasive, electrotherapy addressed as a micro-generated non-thermal waveforms/ ionic currents penetrate targeted structures with complementary therapeutic bases explaining its tertiary benefits on both metabolic or biochemical pathways to restore homeostasis, remodeling extracellular matrix as well promoting cellular regeneration (11-13).
Low level laser therapy (LLLT) is a FDA-approved non-invasive painless, easily applicable therapy with promising results in PJIA children exerting antiinflammatory, antioxidative, and ion bio stimulating therapeutic benefits, also cost-effective modality that facilitates physical functional performance in terms of mobility, swelling and fitness in both acute and chronic pediatric population (14-16).
Recent guidelines for PJIA management focusing on controlling clinical features, structural damage prevention, plus optimizing functional capabilities. Therefore, ensuring previous clinical management algorithm enhances PJIA children development and improves better health-related quality of life, and easier social participation (17).
However, limited clinical trials have been conducted to enhance earlier aggressive rehabilitation that modulate antirheumatic nature of PJIA, or even prohibit PJIA course using novel therapeutic modalities as a new trend to improve physical functional capabilities among JIA children. Thus, the main objective of this study was to compare between pulsed magnetic field versus low level laser therapy in management of polyarticular juvenile idiopathic arthritis.
Material and Methods:
A single prospective clinical, randomized control trial was conducted on forty children with polyarticular juvenile idiopathic arthritis (based on ILAR criteria), were selected from Pediatric Rheumatology Clinic of Tanta university hospital at Gharbia governate, Egypt and The Outpatient Clinc of the faculty of physical therapy Kafr Elsheikh university at Kafr Elsheikh governorate, Egypt also The Outpatient Clinc of the faculty of physical therapy Delta university at Dakahlia governorate, Egypt. Prior to initiating the study, each children parents were signed a consent form before participation in the study. The investigation was carried out in accordance with the ethical standards specified in the 1964 Declaration of Helsinki and received approval from the Research Ethical Committee at the Faculty of Physical Therapy, Kafrelsheikh University, Egypt (No. P.T.REC/ PED /2/2023/40). This trial was registered at Pan African clinical trials registry (No. NCT06226012).
Participants:
Sample size calculation:
In order to detect sample size (n) using the equation 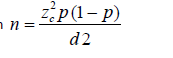
Where α = 0.05, p = 0.000, d = 0.08, σ = 0.0.038
The sample size will equal 40 (20 in each group), If we anticipate a dropout rate.
The eligible participants met the following inclusion criteria: age between 8 and 16 years old of both genders, clinical diagnosis of polyarticular onset of juvenile idiopathic arthritis with involvement of bilateral knee joints, and they received stable medicines in the last three months ‘stable status’ also not participating in a regular exercise program in the last six months.
Patients were excluded if they had any of the following criteria: fixed deformities; history of joint surgery; ankylosing spondylitis or fractures; and/ or bone destruction (erosive changes of the knee joint).
Total sample size was 40 subjects. Patients were randomly assigned to two equal groups. Group A received Pulsed electromagnetic field (PEMF; 15 HZ, 20 G for 15 minutes, 3 sessions per week for successive three months), in addition to traditional exercise program ‘involving strengthening, stretching, proprioceptive, gait and balance training’. Group B received Low intensity laser therapy (LILT; 10 KHZ, 5cm ‘X&Y’ over 25cm2 with 3J/cm2 for 15 minutes, 3 sessions per week for successive three months), in addition to traditional exercise program ‘involving strengthening, stretching, proprioceptive, gait and balance training’.
Instruments
Evaluating instruments
i. Digital goniometer
It is broadly utilized for Pediatric Escola Paulista de Medicina Range of Motion Scale (PEPM-ROM) using a two-legged goniometer. Joint limitation for each motion was classified on a 4-point Likert scale ranging from no -30% limitation in ROM (score range 0-3, total scale 0-6) (18).
ii. Knee Tape measure
It was used to assess the degree of effusion of the affected knee joints (19).
iii. Arabic version of Parent-proxy Childhood Health Assessment Questionnaire (ACHAQ)
It is globally utilized valid and reliable tool used for objective assessment of functional status in children with PJIA in eight areas; dressing and grooming, arising, eating, walking, hygiene, reach, grip, and activities. It was scored on four-point ordinal scale, where 0 represents "no disability", 1 represents ‘some difficulty’, 2 represents ‘much difficulty’ and 3 represents "unable to do".(20)
Treatment instruments:
i. Pulsed electromagnetic field Instrument (PEMFs)
FDA- approved Fisioline s.r.1 Fisiofield Maxi, Verduno, Italy. It was automate calibrated before intervention. This device causes no sounds or sensations for the patient during exposure. The appliance was connected to electrical mains supplying 230 v ± 10% at a frequency of 50 or 60 Hz with earth connection.
ii. Low level laser therapy device (LLLT)
FDA- approved Scanner Bio stimulation Laser unit. Fluorescent contrast was introduced via intra-articular injection of acridine orange (0.5 g/L in 0.9% PBS, 60 mL, 37°C, pH 7.4, 20 min) prior to imaging. Acridine orange (Molecular Probes Inc., Eugene, OR, USA).
Assessment Procedures
i. At the beginning, all demographic data including age, weight, height, and gender were documented, along with screening outcome measures.
ii. Knee range of motion evaluation
Digital goniometer scored on Pediatric Escola Paulista de Medicina Range of Motion Scale (PEPM-ROM) using a two-legged goniometer. Joint limitation for each motion was classified on a 4-point Likert scale ranging from no -30% limitation in ROM (score range 0-3, total scale 0-6).(18)
iii. Knee swelling screening
Tape measurement to assess the degree of effusion of the affected knee joints. It is taken around the knee at level of patella for knee swelling (19).
iv. Functional status evaluation
Arabic version of Parent-proxy Childhood Health Assessment Questionnaire (ACHAQ) was used to evaluate eight functional areas in a score range of 0 ‘no disability’ to 3 ‘’maximum disability’ of participated children with PJIA in a frame over a week.(20)
Treatment procedure
PEMFs therapy for Group (A)
Each child in group (A), has received PEMFs session after approval of caregivers or parents. Then, each was asked to relaxed supine in comfortable clothes with no metallic objects or any sensitive to magnetic field objects. The appliance connected to electrical mains supplying 230V± 10%. The solenoids were adjusted to be over both knee joints. During application, child was asked not to move and remain stable as much as possible. The options of appliance were adjusted with very low 15 HZ, 20 G for 15 minutes, 3 sessions/week for successive 3 months.
Low level laser therapy for Group (B)
Each child in group (B) has received LLLT session after approval of caregivers or parents. Then, each was asked to relaxed supine with semi-flexed knees, while wearing goggles. Treatment parameters were as follows: 10 KHZ, 5cm ‘X&Y’ over 25cm2 with 3J/cm2 for 15 minutes, 3 sessions per week for successive three months.
Traditional physical therapy program for both groups (A& B)
Each child in both groups (A& B) has received the standard physical therapy treatment for PJRA after approval of caregivers or parents. Then, each child has undergone standard physical therapy program that consisted of the Strengthening exercise, stretching exercise, proprioceptive training, gait training, and balance training for one hour per day, three sessions per week.
Statistical analysis
Unpaired t-test was conducted for comparison of subject characteristics between groups. Chi squared test was conducted for comparison of sex distribution between groups. Normal distribution of data was checked using the Shapiro-Wilk test. Levene’s test for homogeneity of variances was conducted to test the homogeneity between groups. Unpaired t-test was conducted for comparison of Knee ROM and circumference, also functional status between groups and paired t-test was conducted for comparison between pre and post treatment in each group. The level of significance for all statistical tests was set at p < 0.05. All statistical analysis was conducted through the statistical package for social studies (SPSS) version 25 for windows (IBM SPSS, Chicago, IL, USA).
Results
Subject characteristics
Table (1) shows the subject characteristics of group A and B. There was no significant difference between groups in age, weight, height, onset and sex distribution (p > 0.05).
| Group A | Group B | p-value | ||
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Age (years) | 11.59 ± 1.39 | 11.15 ± 1.43 | 0.34 | |
| Weight (kg) | 37.21 ± 3.98 | 36.96 ± 4.55 | 0.85 | |
| Height (cm) | 139.48 ± 7.01 | 139.28 ± 7.28 | 0.93 | |
| Onset of disease (years) | 8.80 ± 0.70 | 8.51 ± 0.62 | 0.17 | |
| Sex | ||||
| Girls | 16 (80%) | 16 (80%) | 1 | |
| Boys | 4 (20%) | 4 (20%) |
SD: standard deviation, N: number, %: (percentage), p-value: Probability value
Effect of treatment on Knee ROM and circumference, also functional status:
Within group comparison
There was a significant decrease in VAS and knee circumference at patella and above patella levels post treatment in both groups compared with that pretreatment (p > 0.001). The percent of change in VAS and knee circumference at patella and above patella levels of group A was 78.29, 11.83 and 11.53% respectively and that of group B was 23.97, 4.03 and 18.61% respectively (Table 2).
| Pre treatment | Post treatment | MD | % of change | t- value | p value | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ±SD | Mean ±SD | ||||||||||||||||||
| Knee circumference (cm) | |||||||||||||||||||
| At patella level | |||||||||||||||||||
| Group A | 31.52 ± 1.63 | 27.79 ± 1.79 | 3.73 | 11.83 | 15.45 | 0. 0 0 1 | |||||||||||||
| Group B | 30.72 ± 1.97 | 28.98 ± 1.54 | 1.74 | 5.66 | 4.03 | 0. 001 | |||||||||||||
| MD | 0.8 | -1.19 | |||||||||||||||||
| t-value | -1.39 | -2.24 | |||||||||||||||||
| p 0.17 | p 0.03 | ||||||||||||||||||
| Above patella level | |||||||||||||||||||
| Group A | 32.18 ± 1.56 | 28.47 ± 2.04 | 3.71 | 11.53 | 23.86 | 0.001 | |||||||||||||
| Group B | 31.84 ± 1.61 | 29.90 ± 1.86 | 1.94 | 6.09 | 18.61 | 0.001 | |||||||||||||
| MD | 0.34 | -1.43 | |||||||||||||||||
| t-value | 0.69 | -2.32 | |||||||||||||||||
| p 0.49 | p 0.02 | ||||||||||||||||||
| ACHAQ | |||||||||||||||||||
| Group A | 1.55 ± 0.25 | 0.75 ± 0.65 | 0.8 | 1.34 | 36.27 | 0.001 | |||||||||||||
| Group B | 1.50 ± 0.3 | 1.10 ± 0.5 | 0.4 | 0.67 | 12.72 | 0.001 | |||||||||||||
| MD | 0.05 | -0.35 | |||||||||||||||||
| t-value | -1.26 | -4.07 | |||||||||||||||||
| p 0.21 | p 0.001 | ||||||||||||||||||
SD: Standard deviation; MD: Mean difference; p value: Probability value; ACHAQ: Arabic version of Childhood Health Assessment Questionnaire.
There was a significant increase in knee flexion and extension ROM post treatment in both groups compared with that pretreatment (p > 0.001). The percent of change in knee flexion and extension ROM of group A was 23.84 and 16.97% respectively and that of group B was 13.92 and 13.72% respectively (Table 3).
Between group comparison
There was a significant decrease in knee circumference at and above patella and functional status of group A compared with that of group B post treatment (< 0.001), (Table 2).
There was a significant increase in knee flexion and extension ROM of group A compared with of group B post treatment (<0.05), (Table 3).
| Pre treatment | Post treatment | MD | % of change | t- value | p value | |
|---|---|---|---|---|---|---|
| Mean ±SD | Mean ±SD | |||||
| Knee flexion ROM (degrees) | ||||||
| Group A | 94.05 ± 2.29 | 116.47 ± 2.05 | -22.42 | 23.84 | -32.27 | 0. 001 |
| Group B | 94.97 ± 1.30 | 108.19 ± 2.55 | -13.22 | 13.92 | -18.4 | 0. 001 |
| MD | -0.92 | 8.28 | ||||
| t-value | -1.55 | 11.30 | ||||
| p 0.13 | p 0.001 | |||||
| Knee extension ROM (degrees) | ||||||
| Group A | 104.18 ± 2.33 | 121.86 ± 3.84 | -17.68 | 16.97 | -20.84 | 0. 001 |
| Group B | 103.68 ± 1.30 | 117.91 ± 3.15 | -14.23 | 13.72 | -19.64 | 0. 001 |
| MD | 0.5 | 3.95 | ||||
| t-value | 0.83 | 3.56 | ||||
| p 0.41 | p 0.001 | |||||
SD: Standard deviation; MD: Mean difference; p value: Probability value.
Discussion
Worldwide children with PJIA have a potential consequence on their physical incapacity that restricts gait development. Such physical dysfunction requires a multidisciplinary management team, to overcome daily activities, owing painful nature, knee swelling, also morning stiffness (21).
Clinical practitioners and researchers have a propensity to adopt complementary, non-pharmacological, and less invasive modalities with negligible side effects (22). Pulsed electromagnetic fields, low-level laser therapy, and ultrasound-guided radiofrequency ablation of genicular nerves in conjunction with exercise therapy with both modalities showing promise as strong therapies for arthritic pain (23).
This study was conducted to compare between pulsed magnetic field versus low level laser therapy in management of polyarticular juvenile idiopathic arthritis.
According to current study`s findings, there was a significant increase in knee flexion and knee extension ROM of group A (pulsed magnetic field) post treatment compared with pretreatment. There was a significant decrease in knee circumference at, and above patella level, also a significant decrease of values of ACHAQ indicating improved functional status of group A (pulsed magnetic field) post treatment compared with pretreatment.
Supporting our results, Elboimâ??Gabyzon and Nahhas. Had conducted a singleblinded assessor, randomized, controlled clinical trial on 40 participants aged between 50 and 75 years with grade 2-3 symptomatic knee osteoarthritis. Participants were randomly divided into two groups; PEMFs group, LLLT group. They reported that Western Ontario and McMaster Universities Osteoarthritis index, and stuffiness subscale were significantly lower post treatment compared with pretreatment in pulsed magnetic field therapy group (24).
In agreement with our results, Yang et al. performed a systematic review and meta-analysis of randomized placebo-controlled trials with sixty clinical trials in systematic review and fifteen clinical trials with complete data were included in the meta-analysis. They reported that there was a beneficial effect of pulsed electromagnetic field therapy on stiffness and physical function (25).
Fortunately, Markovic et al. conducted a systematic review of systematic reviews on sixty-nine clinical trials and documented that the use of PEMF is a safe and noninvasive therapy that can lead to improvements in physical function (26).
Also, Eid and Aly. Found that knee flexion and knee extension increased significantly post treatment compared with pretreatment in pulsed electromagnetic field therapy group for hemophilic knee arthropathy. Also, they found that there was a significant decrease in knee circumference at patella level and above patella level in pulsed magnetic field therapy group post twelve weeks of treatment compared with pretreatment (27).
A recent investigator-masked study that was conducted by Elnaggar et al. on forty-eight child suffering from juvenile idiopathic arthritis, with bilateral knee joint involvement, their age ranged from 8 to 16 years old. Participants were randomly allocated to either the low-level laser therapy group (for the treatment by low level laser therapy plus standard physical exercises) or the control group (for the treatment by standard physical exercises). They showed significant improvement post treatment in combined with exercise in terms of fatigue perception, and functional performance (14).
In the current study, there was a significant increase in knee flexion and knee extension ROM of group B (low level laser therapy) post treatment compared with pretreatment. There was a significant decrease in knee circumference at patella level and above patella level in group B post treatment compared with pretreatment. As well, there was a significant decrease in VAS of group A (pulsed magnetic field) compared with that of group B (low level laser therapy) post treatment.
The potential mechanisms that might account for the observed results include the physiological improved microcirculation, ischemia remediation, also mitigation of oxidative stress, as well activating of bioenergetics system by pulsed electromagnetic field (28).
In earlier clinical trial conducted by Zaky and Atya. who carried out a prospective randomized study on thirty juvenile rheumatoid arthritis children their age range was 8-12 years old. Their study group had received pulsed low frequency magnetic field therapy, and had revealed statistically significant improvements in both joint mobility and functional disability variables (29).
In disagreement with our results, Leal-Junior et al. who conducted an earlier systematic review on low-level laser therapy as a phototherapy approach on exercise performance and they stated that significant variation among PJIA is muscular application differs in case of articular low level laser application thus could explain limited therapeutic benefits than electromagnetic therapy (30).
Conclusion
In management of juvenile idiopathic arthritis, both pulsed magnetic field and low-level laser therapy are effective in reducing swelling and increasing knee mobility, and improving overall functional status with superiority of pulsed magnetic field compared to low level laser therapy.
Limitations
A single center, on small sample population with no placebo group, and restricted follow up could enumerated as current study limitations.
Acknowledgement
The authors wish to thank the children and their families who agreed to participate in the study.
Conflict of interest
No potential conflict of interest was reported by the authors.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sector.
References
Handa R and Handa R. (2021). Juvenile Idiopathic Arthritis. J Clin Rheumatol. 99-102.
Dave M, Rankin J, Pearce M and Foster HE. (2020). Global prevalence estimates of three chronic musculoskeletal conditions: club foot, juvenile idiopathic arthritis and juvenile systemic lupus erythematosus. Pediatr Rheumatol Online J. 18(1):49-59.
Mostafa EW, Bakry Abdul-sattar A and Abo Elsaud Dawa G. (2019). Prevalence and factors of functional disability in patients with juvenile idiopathic arthritis. ZUMJ. 25(3):456-463.
El Miedany Y, Salah S, Lotfy H, El Gaafary M, Abdulhady H, Salah H, et al. (2022). Updated clinical practice treat-to-target guidelines for JIA management: the Egyptian College of Pediatric Rheumatology initiative. Egyptian Rheumatology and Rehabilitation. 49(1):27-43.
Saad N, Onel K. (2020). Overview of Juvenile Idiopathic Arthritis. The Open Orthopaedics Journal. 14:101-109.
Ravelli A, Minoia F, Davì S, Horne A, Bovis F, Pistorio A, et al. (2016). Classification Criteria for Macrophage Activation Syndrome Complicating Systemic Juvenile Idiopathic Arthritis: A European League Against Rheumatism/American College of Rheumatology/Paediatric Rheumatology International Trials Organisation Collaborative Initiative. Arthritis Rheumatol. 68(3):566-76.
El-Refaey AM, Sobh NN, Shahin D, Darwish A. (2022). The epidemiological profile of juvenile arthritis: Single center study in Delta region of Egypt. Res Square. 10: 21203.
Abdelaleem EA, Ezzat DA, Mostafa GR. (2021). Functional disability and health-related quality of life in juvenile idiopathic arthritis children from Beni-Suef. Egy Rheumatol Rehabil. 12: 48-56.
Davies R, Gaynor D, Hyrich KL, Pain CE. (2017). Efficacy of biologic therapy across individual juvenile idiopathic arthritis subtypes: A systematic review. Semin Arthritis Rheum. 46(5):584-593.
Onel KB, Horton DB, Lovell DJ, Shenoi S, Cuello CA, Angeles-Han ST et al. (2022). American College of Rheumatology Guideline for the Treatment of Juvenile Idiopathic Arthritis: therapeutic approaches for oligoarthritis, temporomandibular joint arthritis, and systemic juvenile idiopathic arthritis. Arthritis Care Res (Hoboken). 74(4):521-537.
El-Shamy SM, Mohamed AA. (2013). Efficacy of low frequency pulsed electromagnetic field therapy on physical fitness in juvenile rheumatoid arthritis: a randomized, placebo-controlled study. Eng Health. 11:123-127.
Hu H, Yang W, Zeng Q, Chen W, Zhu Y, Liu W. (2020). Promising application of Pulsed Electromagnetic Fields (PEMFs) in musculoskeletal disorders. Biomed Pharmacother. 131:199-201.
Luigi C, Tiziano P. (2020). Mechanisms of action and effects of pulsed electromagnetic fields (PEMF) in medicine. J Med Res Surg. 1(6):1-4.
Elnaggar RK, Mahmoud WSE, Kamal W, Alqahtani B, Alrawaili SM, Elfakharany MS. (2022). Low-energy laser therapy application on knee as an auxiliary treatment in patients with polyarticular juvenile idiopathic arthritis: a dual-arm randomized clinical trial. Laser Med Sci. 37:1737-1746.
Zhang R, Qu J. (2023). The mechanisms and efficacy of photobiomedulation therapy for arthritis: A comprehensive review. Int J Mol Sci. 24(18): 14293-14312.
Yudoh K, Karasawa R. (2018). Effects of low-level laser therapy on clinical characteristics and laboratory profiles in synovitis in patients with rheumatoid arthritis. Nov Tech Arth Bone Res. 2(5): 1-8.
Shoop-Worrall SJW, Verstappen SMM, McDonagh JE, Baildam E, Chieng A, Davidson J et al. (2018). Long-term outcomes following achievement of clinically inactive disease in juvenile idiopathic arthritis: the importance of definition. Arthritis Rheum 70:1519-1529.
Lind V, Svensson M, Harringe ML. (2021). Reliability and validity of a digital goniometer for measuring knee joint range of motion. Measur Phys Edu Exer Sci. 26(3): 191-198.
da Silva AEL, Martimbianco ALC, Pontin JCB, Lahoz GL, Filho MC, Chamlian TR. (2014). Reproducibility analysis of knee circumference in individuals with osteoarthritis. Acta Fisiatr. 21(2):49-52.
Madi SM., Al-Mayouf SM., Grainger CG., Bahabri SA. (2004). The Arabic version of childhood health assessment questionnaire modified for Arabic children. Saudi Med J. 25(1): 83-87.
Sudhakar M, Kumar S. (2024). Juvenile Idiopathic Arthritis. Indian J Pediatr. 1-10.
de Sire A, Lippi L, Curci C, Calafiore D, Cisari C, Ammendolia A, et al. (2021). Effectiveness of combined treatment using physical exercise and ultrasound-guided radiofrequency ablation of genicular nerves in patients with knee osteoarthritis. Appl Sci [Internet]. 2021; 11(10).
Mansouri V, Arjmand B, Rezaei Tavirani M, Razzaghi M, Rostami-Nejad M, Hamdieh M. (2020). Evaluation of efficacy of low-level laser therapy. J Lasers Med Sci. 11(4):369-380.
Elboim-Gabyzon M, Nahhas F. (2023). Laser therapy versus pulsed electromagnetic field therapy as treatment modalities for early knee osteoarthritis: a randomized controlled trial. BMC Geriatr. 23(1):144.
Yang X, He H, Ye W, Perry TA, He C. (2020). Effects of pulsed electromagnetic field therapy on pain, stiffness, physical function, and quality of life in patients with osteoarthritis: A systematic review and meta-analysis of randomized placebo-controlled trials. Phys Ther. 100(7):1118-1131.
Markovic L, Wagner B, Crevenna R. (2022). Effects of pulsed electromagnetic field therapy on outcomes associated with osteoarthritis. Wien Klin Wochenschr.134(11):425-433.
Eid MA, Aly SM. (2015). LASER versus electromagnetic field in treatment of hemarthrosis in children with hemophilia. Lasers Med Sci. 30(8):2179-2187.
Fiani B., Kondilis A., Runnels J, Rippe P and Davati C. (2021). Pulsed Electromagnetic Field Stimulators Efficacy for Noninvasive Bone Growth in Spine Surgery. J Korean Neurosurg Soc. 64(4):486-494.
Zaky NA, Atya AM. (2014). Effect of pulsed low frequency magnetic field on balance and ankle function in patients with juvenile rheumatoid arthritis. Middle East J Sci Res. 21:1848-1854.
Leal-Junior ECP, Vanin AA, Miranda EF, de Carvalho PdTC, Dal Corso S, Bjordal JM. (2015). Effect of phototherapy (low-level laser therapy and light-emitting diode therapy) on exercise performance and markers of exercise recovery: a systematic review with meta-analysis. Lasers Med Sci 30(2):925-939.