Research Article - (2023) Volume 18, Issue 6
Extracorporeal Shockwave Therapy And Placebo Control For Insomnia Within Diabetic Neuropathy
Engi E. Sarhan1*, Nermeen Bleedy2, Sally Mosad Kamar3, Nesma EM. Barakat4, Shaimaa E Salem5 and Amr Ali Ali Elkhodary6*Correspondence: Engi E. Sarhan, Lecturer of Physiotherapy for Neurology and Its Surgery, Faculty of Physical Therapy, Kafrelsheikh University, Egypt, Email:
2Physical Therapy Department, College of Applied Medical Sciences, Jerash University, Jerash, Jordan
3Lecturer in Physical Therapy Department for Integumentary Disorders, Faculty of Physical Therapy, Kafrelsheikh University, Egypt
4Lecturer of Physical Therapy for Pediatrics, Faculty of Physical Therapy, Kafrelsheikh University, Egypt
5Lecturer of Physical Therapy in Basic Science Department, Faculty of Physical Therapy, Cairo University and Al Ryada University for Science and Techno, Egypt
6Lecturer of Physical Therapy for Internal Medicine and Geriatrics, Faculty of Physical Therapy, Kafrelsheikh University, Egypt
Received: 09-Dec-2023 Accepted: 15-Dec-2023
Abstract
Purpose: To allocate the influence of extracorporeal shockwaves on insomnia in comparison to placebo control in patients with a complaint of diabetic neuropathy. Methods: According to inclusion and exclusion items of the study, one hundred twenty six patients participated randomly into two equal groups, (study group) was the extracorporeal shockwave (ESW) group; (control group) was placebo receiver one. Both groups had been treated once a week for three months.
Results: Outcomes established that patients in the study group had improved in foot neuropathic pain and insomnia severity; there were a significant difference between groups (p > 0.05). Conclusion: ESWT could be recommended for rehabilitation to improve the diabetic neuropathic foot pain and the severity of insomnia.
Keywords
Extracorporeal Shockwave Therapy. Diabetes Mellitus Type 2. Neuropathic Pain. Insomnia
Introduction
While someone struggles with falling asleep or waking up sin the early morning three times per week or more in a single month, he/she has insomnia1. Nowadays, many in the general population are facing sleep disorders. Insomnia (chronic difficulty sleeping with or without repetitive waking up early) is the most recurrent sleep disorder (30–40%)2. Diabetes mellitus affects 415 million people live with the disease, with a 5% annual increase, resulting in at least half a billion people living with the disease in 20453. The most prevalent complication of diabetes is poly-neuropathy (symmetrical diminished followed by loss of sensation in the extremities, which starts in the longer nerves and distally) 4. Unfortunately, more than half of diabetic patients have diabetic polyneuropathy 4. An abundance of adult patients with diabetic neuropathy (DN) have insomnia, A marked number of DM patients suffer from insomnia, with a prevalence of 39% due to many smitten body functions (neurologic, metabolic, and endocrine) leading to pain, burning sensation, uncomfort and tingling due to atherosclerosis of the micro-vessels (vasa nervosa) of nerves, causing chronic nerve inflammation2. Blockade of diabetic neuropathy is necessary to recover from insomnia3. Extracorporeal shockwave therapy (ESWT) is considered a non-invasive intervention that overcomes DN via controlling pain and stimulating healing5. It is characterized by a wide range of acoustic energy. Waves, focused or radial. Its energy flux density unit is (EFD, MJ/mm²)6. Consequently, the ESWT scope is from (0.001 to 0.5 MJ/mm²)6. ESWT has a small single pulse width of 0–30 ms, a wide frequency (0–20 MHz), and a high pressure amplitude (0–120 Mpa) 6. All of the previous mentioned features affect nociceptive impulses via gate control theory, change the chemical medium around the nerve, demean inflammatory mediators, and eliminate free nerve ending irritation6. It is predicted that ESWT has a fluffy effect on the affected nerves, increasing expression of activating transcription factor 3 (ATF-3) and of growth-associated phosphoprotein 43 (GAP-43) in dorsal root ganglion neurons (reaching cell body also)7. Wu Y T and his colleagues excluded that, shockwave therapy of radial form could subside pain and enhance range of motion of hand joints in those cases of peripheral neuropathy (carpal tunnel syndrome)8. On the other hand, these resulting insomnia symptoms lead to a deterioration of glucose tolerance and insulin sensitivity3. Jung H.L and Sung H.C deduced that ESWT relieves pain from peripheral nerve degeneration (sciatic nerve), encourages muscle power, and overcomes hypertonia9. Samantah B.J et al concluded that sleep manifestations are very common in diabetic patients, having a bad influence on health outcomes. They found that management of the sleep disturbance could stop diabetes's progressive course, which will ultimately promote general health and life quality10. A safe, long-term effective and convenientcost modality of treatment is extracorporeal shockwave therapy (ESWT), which has been estimated for improvement of the symptoms of insomnia in DN patients due to its regenerative biological influence4. Improvement in DN depends on controlling neuropathic pain. ESWT controls it via conjugation of integrin molecules (growth cone on nerve axon membrane) with a lot of extracellular molecules, production of Schwann cells in the degeneration site and stimulation of macrophages10.
Patients and methods
Participants
A study sample of 126 patients (80 males and 46 females) (66 Rt foot and 69 Lt foot) were recruited from outpatient clinic of Kafrelsheikh University hospital and enrolled according to their eligibility to participate in this study. All patients are suffering from insomnia and diabetic neuropathic pain.
They all included in the following criteria, All patients diagnosed with neuropathic foot due to diabetes mellitus (DM) type II (HBA1C was less than 7.5) and insomnia (according to the insomnia severity index). The BMI of all patients was class II (25-30). The patients' ages ranged from 40 to 60 years old.
Patients with some conditions had been excluded as follows: Other neurological conditions include neuropathy caused by drug or alcohol abuse and sensory impairments caused by lumbar disc prolapse for focusing on neuropathy in diabetic patients. Deformities (Charcot foot) that might interfere with the results. Complaining of nephropathy Patients with clotting disorders as ESWT affects circulation directly. Corticosteroids six months before the recruitment period to be sure that the effect of our treatment. Also, we excluded patients those are suffering from associated psychological disorders such as depression to keep them co-operative with us in the study period. Patients suffering from obstructive sleep apnea did not share in this study to avoid bias that originates from other sleep disorders. Anyone who has received ESWT previously for any reason for blinding reason. Finally, patients who are suffering from diabetic foot ulcers couldn't be included.
All participants (males and females) had been checked corresponding to inclusion and exclusion criteria. Whole, competent patients signed an evident consent form before their participation in this study. All participants had been chopped randomly and equally [1:1] (simple randomization) into two groups: study group (1) and control group (2).
Ethical committee of faculty of physical therapy Kafr-elsheikh University approved the protocol of this study. The Guidelines of Declaration of Helsinki on the conduct of human research 1975 are the guidelines that this study based on.
Instrumentation
Assessment tools
Each patient (in both groups) had been evaluated before the intervention and after 3 months (the treatment end point) by the same therapist using:
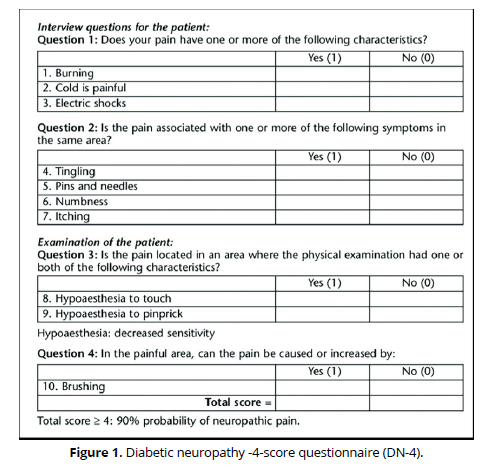
Diabetic neuropathy-4-score questionnaire (DN-4) (Figure 1) which is a scale of 4questions, including 10 sub-questions with a score of 10, if patient's score is ≥4, the diagnosis is DN (as a primary outcome) 11.
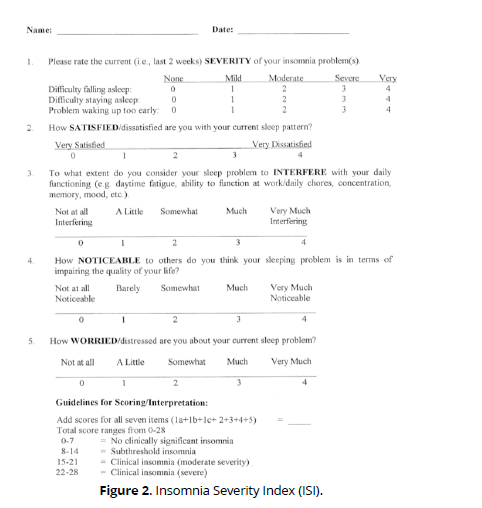
Insomnia Severity Index (ISI) (Figure 2) which is a 7-item self-reported questionnaire to measure the quality, intensity, and influence of insomnia (final score is explicated as follows: 0-7 no insomnia, 8-14 mild insomnia, 15-21 moderate insomnia and 22-28 severe insomnia) (as a secondary outcome) 12.
Treatment tools
The model of ESWT equipment that we used is EMS-SWISS DOLORCLAST MASTER. Radial pressure wave - Swiss made from the inventors of radial shock wave therapy. FDA approved. Features of it as follows: Colour touch screen display, easy to master with its preset protocols, accurate manual settings, pressure ramp-up and energy density display. It can Inform the patients using treatment pictures, videos and method details. Also can Track clinical results by recording patient's data. The Specifications of this ESWT machine are: Frequency range: 1 - 20 Hz, in 1Hz increments, air pressure range: 1.5 - 4 bar (increment of 0.1 bar) and impulse range: 500 – 10000 (increment of 500 impulses).the machine included: Swiss DolorClast® Master console, evo Blue® handpiece, contact gel, trolley cart and external compressor (Figure 3).
Therapeutic procedures
Patients in group 1 was in a relaxed supine lying position and received the application on the mid-dorsum of the foot with parameters of 1000 impulses (0.08 mJ/mm, 2.4 Hz) 13. Patients in group 2 received ESWT placebo treatment that is installed on the equipment's software (provided just sounds without any real parameters). Accordingly, all patients in both groups received treatment once a week for a three-month long period by the same therapist. We achieved double blind control as follows: informed the patient and therapist that the treatment will be to prevent diabetic foot ulcer.
Sample size and data analysis
According to the results of a pilot study that we performed, the mean and standard deviation of DN-4 were 4.78 ±1.9 and 2.6 ±1.58 for group 1 and group 2. As a result, we used the G*power software to compute the sample size (n) for two independent means with an alpha error of 0.05 and a power of 95%: n = 126 for both groups, 63 for each. Regarding this study, we decided to perform: a-Chi Square Analysis Test for demographic data (sex) and an independent t-test for age, illness duration, and daily times of hypoglycemic drug intake. b- A parametric one-tailed t-test (for comparing means of DN-4 and ISI score in both groups). A paired t-test was for intra-group but an independent t-test was for inter-groups (before intervention and after). The significance level was 0.05 (p value) and the confidence interval is 95%.
Results
Demographic data
Table 1 showed the mean ± SD age of group 1 and 2. There was no significant difference between both groups in the mean age (p = 0.599). Also, there was no significant difference in sex distribution between groups (p = 0. 459). Also there was non-significant difference between illness duration (p = 0.681) and daily times of hypoglycemic drug intake between both groups (p = 0.681).
| Group 1 | Group 2 | t value | P value | |
|---|---|---|---|---|
| Age | 50.78, ±4.8 | 51.24,±4.90 | 0.5279 | 0.599 |
| Illness duration | 8.38, ±2.51 | 8.56, ±2.24 | 0.4117 | 0.681 |
| Daily times of hypoglycemic drug intake | 1.67, ±0.57 | 1.62, ±0.49 | 0.5041 | 0.6151 |
| Sex | 38/25 | 42/21 | χ2 value | 0. 459 |
| Male/female | 0.548 |
Effect of treatment on DN-4 and ISI
Paired t test revealed that, there was significant difference in mean value of DN-4 in group 1 before and after treatment (t = 10.3) (p= 0.0001) (CI=0.95)
and also extremely statistical significant difference in mean values of ISI in group 1 before and after treatment (t = t = 11.15) (p= 0.0001) (CI=0.95). according to group 2 we neither detected significant difference in mean values of DN-4 before and after treatment nor detected in mean values of ISI (t = 0.87) (p= 0.3868) (CI= 0.95), (t = 1.9565) (P= 0.0549) (CI= 0.95). Table 2
| G1 | G2 | P value | |
|---|---|---|---|
| DN-4 before | 6.48, ±1.51 | 6.73,±1.71 | 0.4411 |
| DN-4 After | 4.9, ±1.99 | 6.48, ±1.72 | 0.0001* |
| P value | 0.0001* | 0.3868 | |
| ISI before | 16.67, ±4.17 | 17.62, ±4.78 | 0.2185 |
| ISI after | 14.29,± 4.89 | 17.1,±5.29 | 0.0018* |
| P value | 0.0001* | 0.0549 |
By fulfillment of independent t-test we concluded that, for group 1 and 2 there was no significant difference between DN-4 mean values nor ISI mean values before treatment (t = 0.7728) (p = 0.4411) (CI= 0.95), (t = 1.2367) (p = 0.2185) (CI= 0.95).
On the other hand there was an extremely statistically significant difference in mean values of DN-4 between group 1 and 2 after treatment (t = 4.3541) (p = 0.0001) (CI=0.95). As for the ISI mean values of group 1, 2 after treatment we found a very statistically significant between them (t = 3.1818) (p = 0.0018) (CI= 0.95) (Table 2).
Discussion
This study has been take place to illustrate the difference between ESWT and placebo control in the treatment of insomnia in diabetic patients those are suffering from neuropathy. Our findings illustrated that in the study group there is significant difference in the severity of insomnia and in neuropathic foot pain according to ISI and DN-4scoring after intervention in comparison to pre-treatment (0.0001), (0.0001). This is perhaps due to the physiological effect of shock wave therapy intra and extracellular effects, such as protein synthesis, pain relief, re-vascularization, cellular proliferation, neuro and chondroprotection leading to tissue renewal and improving functions of injured tissues and relaxation so, causing improvement of sleep quality. Our findings are harmonious with Claudio and his colleagues, they extrapolated that ESWT is a regenerative relaxing medical technique for treatment of many soft tissue injuries14.
In control group there is no significant difference in level of insomnia according to ISI scoring (0.054) and in neuropathic pain according to DN4 scoring (0.386) after treatment in comparison to pre-treatment. We estimated that the cause of this minimal change is that placebo analgesic and relaxing effect is linked to endogenous opioid system via psychological mechanisms verbally induced expectancies, cued and contextual conditioning and social learning. This finding is on the same track with Colloca et al. who concluded that placebo causes lowering in some brain area activity as prefrontal, thalamus, anterior cingulate cortex and insula. It also involves the descending pain modulating system causing some sort of analgesia15.
On the opposite side, Nalan et al. concluded that, the ESWT does not seem to be of higher effect either in pain relief or enhancing body functions at least for three months follow up16.
By comparing between study and control group we concluded that there is significant difference in reducing insomnia severity and neuropathic pain after treatment (0.001) (0.0001). This is may be due to ESWT can elevate permeability of cells, activates cellular division and accelerates rate cytokine production. Sensitive cells to mechanical stimulation as macrophages can be activated by shock waves. ESWT is estimated producing shear force that stimulate capillary inner walls. Cells in those walls (endothelial and smooth muscle cells) were responding to this shearing stress by releasing nitric oxide and vascular endothelial growth factors resulting in improving blood flow and relaxing blood vessels as immediate effect and stimulates angiogenesis as long lasting stimulation effect (delayed effect). Our results are consistent with results of Anna et al. as they concluded that, extracorporeal shock waves therapy improves nitric oxide synthase production of growth factors and thus has immediate and prolonged effect on chronic pain and normal functions17.
Limitations of the study
• Self-reported data as ISI and DN-4 are subjective and depending on each patient.
• Lack of prior research studies on this topic
Conclusion
Application of ESWT was significantly effective in decreasing insomnia severity and neuropathic pain in diabetic patients those suffering from neuropathy. The percentage of group (A) improvement is about 80% over group (B).
Author’s contributions
All of authors were fully involved in drafting this article and approved the submission of the final version for publication.
Ethical approval
Ethical approval was gained from the scientific research ethical committee of physical therapy faculty, Kafr-elsheikh University (No P.T/NEUR/1/2023/23)
Funding
Both authors provided the financial issue for this research by themselves, with no financial support from any one.
Declaration of competing interest
The authors declare no conflict of interest as this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
Thomas Roth, 2007. Insomnia: Definition, Prevalence, Etiology, and Consequences. Journal of clinical sleep medicine, 3(5), pp.7-10.
Marc A. Paantjens, Pieter H. Helmhout, Frank J. G. Backx, Faridi S. van Etten‑Jamaludin and Eric W. P. Bakker, 2022. Extracorporeal shockwave therapy for Mid‑portion and insertional achilles tendinopathy: A Systematic Review of Randomized Controlled Trials. Sports medicine journal, 12(6), pp.48-69.
Nigel A. Calcutt, 2020. Diabetic neuropathy and neuropathic pain: a confusion of pathogenic mechanisms? HHSJ, 161(1), pp.65-86.
Eva L. Feldman, Brian C. Callaghan, Rodica Pop-Busui, Douglas W. Zochodne, Douglas E. Wright, David L. Bennett, Vera Bril, James W. Russell and Vijay Viswanathan, 2020. Diabetic neuropathy. HHSJ, 5(1), pp.42-82.
Karine Spiegel, Kristen Knutson, Rachel Leproult, Esra Tasali and Eve Van Cauter, 2008. Sleep loss: a novel risk factor for insulin resistance and Type 2 diabetes. Journal of Appl Physiol, 463(1), pp.139-160.
Dunya Tomic, Jonathan E. Shaw and Dianna J. Magliano, 2022. The burden and risks of emerging complications of diabetes mellitus. Nature reviews endocrinology journal, 13(2), pp.1-15.
Thomas Roth, Catherine Coulouvrat, Goeran Hajak, Matthew D. Lakoma, Nancy A. Sampson, Victoria Shahly, Alicia C. Shillington, Judith J. Stephenson, James K. Walsh and Ronald C. Kessler, 2012. Prevalence and perceived health associated with insomnia based on DSM-IV-TR; international statistical classification of diseases and related health problems, tenth revision; and research diagnostic criteria/international classification of sleep disorders, second edition criteria: results from the america insomnia survey. Socity of biological psychiatry journal, 69(2), pp.592-600.
Paolo Sanzo, 2012. The Physiological effects of extracorporeal shockwave therapy in the treatment of plantar fasciitis and other musculoskeletal conditions. Sports medicine journal, 59(10), pp.1123-1134.
Jung-Ho Lee and Sung-Hyoun Cho, 2013. Effect of extracorporeal shock wave therapy on denervation atrophy and function caused by sciatic nerve injury. J. Phys. Ther. Sci., 25(9), pp.1067-1069.
Samantha B. J. Schipper, Maaike M. Van Veen, Petra J. M. Elders, Annemieke van Straten, Ysbrand D. Van Der Werf, Kristen L. Knutson, Femke Rutters, 2021. Sleep disorders in people with type 2 diabetes and associated health outcomes: a review of the literature. Diabetologia journal, 64(8), pp.2367-2377.
Josie Carmichael, Hassan Fadavi, Fukashi Ishibashi, Angela C. Shore and Mitra Tavakoli, 2021. Advances in Screening, Early Diagnosis and Accurate Staging of Diabetic Neuropathy. Frontiers in endocrinology journal, 12(5), pp.789-801.
Charles M. Morin, Geneviève Belleville, Lynda Bélanger and Hans Ivers, 2011. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. sleep journal, 34(5), pp.601-608.
Thomas Haunser and Antal Nogradi, 2013. The use of shock waves in peripheral Nerve regeneration: new perspectives? The international review of neurobiology, 109(12), pp.85-98.
Wu Y T, Ming Jen K, Yu-Ching C, Chih-Ya C, Ching Y L,Tsung-Y L, Feng-M S and Liang Cheng C, 2015. Effect of radial shock wave therapy for carpal tunnel syndrome: A prospective randomized, double-blind, placebo-controlled trial. Journal of orthopedic research, 34(6), pp.977-984.
Claudio Lopes Simplicio, Joseph Purita, Willum Murrell, Gabriel Silva Santos and Rafael Santos, 2020. Extracorporeal shock wave therapy mechanisms in muscloskeletal regenerative medicine. Journal of Clin Orthop Trauma, 11 (3), pp. 380-389.
Nalan Capan, Sina Esmaeilzadeh, Aydan Oral, Ayse Karan and Dilsad Sindel, 2016. Radial extracorporeal shock wave therapy is not more effective than placebo in the management of lateral epicondylitis: Adouble-blind, Randomized, placebo-controlled trial. Am J Phys Med Rehabil, 95(7), pp. 495-506.
Anna M Larking, Michael Clinton, Mary Hardy and Keith Andrews, 2010. Randomized control of extracorporeal shock wave therapy versus placebo for chronic decubitus ulceration. Clinical rehabilitation journal, 24(6), pp. 222-229