Full Length Research Article - (2023) Volume 18, Issue 5
*Correspondence: Kholoud Sameh Ghoniem, B.Sc., Department of Physical Therapy for Paediatrics, Faculty of Physical Therapy, Cairo University, Egypt, Email:
2Assistant Professor of nutrition, National nutrition institute, Egypt
3Associate Professor of Physical Therapy for Paediatrics, Faculty of Physical Therapy, Cairo University, Egypt
Received: 06-Oct-2023 Published: 20-Oct-2023
Abstract
Background: Over the past 30 years, childhood obesity has increased by 50% globally. Child obesity is a serious public health issue that has the potential to affect a child's osteoarticular health and cause continuous chronic pain. A training program which aims at improving lower limb muscle strength and dynamic balance may be able to improve lower limb musculoskeletal symptoms i.e. pain and discomfort. With a great deal of research on neuromuscular exercises and muscle strengthening. Yet, the majority do not focus on the population of obese children. So, the purpose of this study was to investigate the effect of strengthening and neuromuscular training program on lower limb pain in obese children.
Subjects and methods: Thirty boys and girls aged between 8 and 11 years were enrolled in the study, selected from schools and divided into 2 groups, Control group underwent a weight reduction plan and study group underwent the same weight reduction plan in addition to neuromuscular and strength training exercise program.
Results: There was a significant difference (MD=1.20; P=0.002; P<0.05) in the mean ±SD values of the visual analogue scale (VAS) between the control group and the study group after-treatment (2.40±0.18 and 1.20±0.08, respectively) which was favorable for the study group. There was a significant difference in the mean ±SD values of all lower limb muscle groups power between control group and study group after-treatment which was favorable of study group.
Conclusion: The findings determined that a neuromuscular and strength training exercise program combined with weight reduction for obese children population can increase lower limb muscle strength and reduce pain more significantly than does weight loss alone.
Keywords
Obesity. Children. Strength. Neuromuscular exercise. Pain. Lower extremity
Introduction
Due to the rising prevalence of this condition, obesity represents an international threat (1). Obesity has become a significant public health issue due to the rise in its frequency over the past few decades (2). In 2014, the obesity prevalence in Egyptian children was 14.7 and 15.08% for girls and boys, respectively (3).
The likelihood of musculoskeletal and joint pain will likely increase in obesity due to higher mechanical demands on the body. Higher body mass index (BMI) has been linked to greater musculoskeletal discomfort, especially in the lower limb, according to a number of research studies (4). Higher pressures inside articulating joints like the knee and ankle primarily causes the overweight and obese children to experience musculoskeletal pain (5,6).
In a recent scientific study estimating the locations of musculoskeletal pain in children and adolescents aged 2 to 19, severely obese children's lower extremities were shown to experience musculoskeletal pain more frequently than children with normal Body Mass index (BMI) (7). The chronic musculoskeletal pain of the lower extremities was located in the knees, ankle joints (8-10).
Pain and various orthopaedic problems, which can restrict physical activity, might also be linked to biomechanical alterations in bony alignment (5).
Thivel et al concluded that there is compelling evidence that children and adolescents who are obese have lower muscle fitness than their normal weight equivalents (11).
According to Tomlinson et al, obese individuals have reduced maximum muscle strength relative to body mass in their anti-gravity muscles compared to nonobese persons (12). This effect on an obese individual is shown to increase the risk of developing osteoarthritis (13) and lead to functional restrictions (14).
Evidence suggests that high levels of adipose tissue hinders the agonist muscle contraction causing limitation in function and low strength relative to body mass (15).
Syed and Davis proposed that obese individuals with lower quadriceps muscular strength compared to body weight have earlier quadriceps muscle fatigue, which diminishes shock absorption and raises knee loading rate and variability during locomotion (17).
Dufek et al stated that In comparison to children of healthy weight, overweight children had significantly slower walking speeds, lower percentages of double support, shorter swing phase times, and wider stances (18).
Even though strength and neuromuscular training have been the subject of numerous research studies, they were not exclusively designed for obese children and adolescents. There is still a lack of high-quality studies that examine the outcomes of such treatments. As a result, the goal of this study is to examine how strengthening and neuromuscular training affects children with obesity regarding lower limb muscle strength and musculoskeletal pain.
Methods
This study was carried out at The Egyptian Ministry Of Education schools. The inclusion criteria were children with ages 8-11 years who scored 95th percentile or greater on the growth chart (obese category), their Visual analogue scale scores were between 3.4 and 6.5 (moderate pain intensity). Children had been suffering from obesity and lower limb musculoskeletal pain for more than 3 months, Calorie intake exceeded 1600 kcal/day for girls and 1800 kcal/day for boys. All participants were able to follow the verbal and visual commands.
The exclusion criteria were children with recent injury or fracture in lower limb through the past six months, malnutrition disorders, diet or anti-inflammatory medications, any musculoskeletal deformity in the lower extremities or trunk and physiological growing pains.
Children were randomly allocated into 2 groups; 15 children for each group.
-The control group underwent a weight reduction plan designed by a nutritionist.
-The study group underwent the same weight reduction plan in addition to six weeks of physical therapy rehabilitation program.
Children and parents were fully informed about the risks and benefits of the procedures. Informed consent was obtained from parents.
Study procedures:
A. Assessment procedures
1. Anthropometric assessment
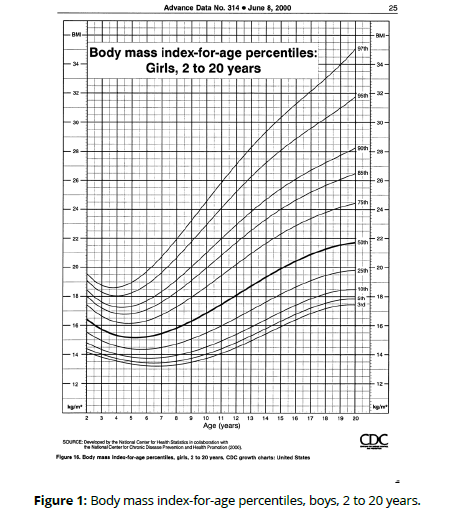
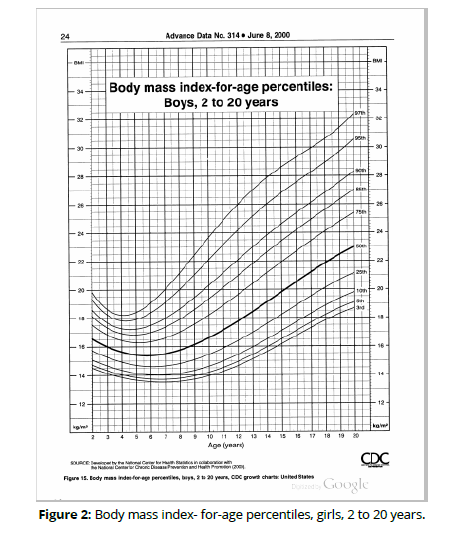
Children were recruited after height and weight assessment to calculate Body Mass Index (BMI). BMI percentile was determined through finding the weight status category for the calculated BMI-for-age percentile using Body mass index -for-age percentiles, boys, 2 to 20 years (figure 1) and Body mass index - for-age percentiles, girls, 2 to 20 years (figure 2). (Figures 1,2)
2. Dietary assessment
24-hour recall method and food frequency questionnaire were used. Frequency questionnaire included all common food items, the amount and frequency of consumption. 24-hour recall included all food items taken during the last 24 hours in a semi quantitative method. Individual food intake was calculated and analysed using computer aided nutritional analysis program of national nutrition institute, Cairo, Egypt
3. Assessment of pain score by visual analogue scale
The child marked on a zero to ten line at the point that they feel represented their pain intensity, a higher score indicates higher pain.
4. Assessment of muscle strength
Muscular strength is measured with a hand-held dynamometer over a range of 0 to 60 Kg-force. According to mentply’s protocol (19), the testing positions utilized to evaluate each muscle group were chosen to ensure that the participants were well stabilized while also limiting the impact of gravity on the measurement. When the subject applied their maximum force against HHD, the examiner kept it still until the subject's maximum muscle effort was achieved and the tested muscles gave way. Using anatomical landmarks, the testing positions and the dynamometer's applying points were established (Table 1).
| Muscle group | Position | Dynamometer placement |
|---|---|---|
| Hip flexion | Sitting and hips and knees flexed at 90°. | anterior aspect of the thigh, proximal to the knee joint |
| Hip extension | Lying prone and hips and knees extended. | posterior aspect of the shank, proximal to the ankle joint. |
| Hip abduction | Lying supine and hips and knees extended. | placed on the lateral aspect of the shank, proximal to the ankle joint |
| Hip adduction | Supine and hips and knees extended. | medial aspect of the shank, proximal to the ankle joint |
| Knee extension | Sitting with hip and knees flexed at 90°. | anterior aspect of the shank, proximal to the ankle joint |
| Knee flexion | Sitting with hips and knees flexed at 90. | posterior aspect of the shank, proximal to the ankle joint |
A- Treatment procedures
1. Nutritional plan
Both groups received a diet plan which concentrated on:
I. Maintaining adequate levels of calorie intake for each child which was calculated according to age using the equation 1000+(age-1)x110 for boys and 1000+(age-1)x100 for girls
II. Calories were divided into is 20% protein, 30% fat, and 50% carbohydrates to meet the nutritional needs.) And delete the rest.
2. Physiotherapy rehabilitation program
The study group received a 6-week neuromuscular training and strengthening exercise in the form of knee/hip joint muscle strength training.
1. Quadriceps strengthening
Weight-bearing and non-weight-bearing exercises were both implemented. We adhered to Lim's quadriceps strengthening plan (17). Three non-weightbearing exercises were performed by the participants at the start to help them adapt to the exercise. Three weeks later, three additional weight-bearing workouts were added. Exercises for the quadriceps were performed in sets of two, progressing as fast as possible to three sets, with ten repetitions in each set. Table 2 lists the quadriceps strengthening exercises. (Table 2)
| 1 | Flexing the hip to 30º, ankle weights were used to give resistance from supine position. |
| 2 | Extension of the knee and a roll under it, ankle weights were used as a resistance from supine position. |
| 3 | Full knee extension beginning at a 90° angle from sitting position, ankle weighs were used as resistance. |
| 4 | Squatting from full extension to 30° of knee flexion, placing a ball against a wall and may be advanced by holding dumbbells in both hands. |
| 5 | Squatting between 40° and 90° of knee flexion with placing a ball between the child’s back and the wall then advancing by holding dumbbells in both hands. |
| 6 | Ascending a stepper with a height of 30 cm. |
Intensity of the exercises were monitored continuously. The training load was adjusted using the One Repetition Maximum (1RM) test which is defined as the maximal weight that can be lifted once, while maintaining the correct lifting technique (21). The 1RM test has been found to be safe across a variety of groups, including those of children, older people, and patients (22, 23)
80% of the 1RM was used as the training load. The 1RM was calculated by gradually increasing the load until child could not lift it while moving through the recommended joint range of motion. Every two weeks, the 1RM was measured in order to modify the training load (24,25).
2. Hip strengthening exercise
The training plan described by Bennell et al (26) was employed to strengthen the hip muscles. There are six exercises in this program that target the hip abductor and adductor muscles. Ten repetitions were done in three sets by all children. Exercises were modified based on the child's capacity to perform10 repetitions. Table 3 lists the implemented exercises. (Table 3)
| 1 | Abduction in side lying, ankle cuff weights were used as resistance. |
| 2 | Abducting the hip in standing unilaterally with the use of a resistance band. |
| 3 | Standing with one shoulder to the wall while performing isometric hip abduction with knee 90° flexed and the other lower limb on the floor. |
| 4 | Clam in side lying position, elastic band was used as a resistance. |
| 5 | Bridging from supine. |
| 6 | Unilateral bridging from supine with 90° of knee flexion in the opposite limb. |
3. Neuromuscular exercises
Balance exercises on one leg and two legs made up the neuromuscular exercises. According to the technique established by Bennell et al (26), participants were given instructions for maintaining more neutral knee alignment during specific tasks to improve the control over their hips and knee to assist in minimizing pain and prevent excessive strains to the joint, knee flexion shouldn't be allowed to go over 30 degrees. Unstable surfaces, like a foam mat or balancing board, were supplied to assure progression. In addition, the number of repetitions was raised along with a variety of movement patterns and training speeds. The progression was tailored on each person's needs in order to reduce pain while exercising. Table 4 provides an overview of the neuromuscular exercises. (Table 4)
| 1 | Standing on both limbs and advancing from a mat to balance board. |
| 2 | Standing on both limbs and advancing from a mat to balance board closing his/her eyes. |
| 3 | Standing on both limbs and advancing from a mat to balance board: two subjects are standing in front of each other throwing and catching a ball. |
| 4 | Static squats, advancing from a mat to balance board. |
| 5 | Static squat on foam surface throwing and catching a ball. |
| 6 | Standing on one leg on a soft surface advancing from a mat to balance board. |
| 7 | Standing on one leg, advancing from a mat to balance board and their eyesight is covered. |
Statistical Analysis
The statistical analysis was conducted by using the statistical SPSS Package program version 25 for Windows (SPSS, Inc., Chicago, IL). The following statistical procedures were conducted:
- Quantitative descriptive statistics data including the mean and standard deviation for children demographic data (age and BMI), pain and muscle strength, variables.
- Qualitative descriptive statistics data including the frequency and percentage for children gender variable.
- Multivariate analysis of variance (MANOVA) used to compare the tested major dependent variables of interest (pain and muscle strength) at different tested groups and measuring periods. Mixed design 2 x 2 MANOVA-test was used, the first independent variable (between subject factors) was the tested groups with 2 levels (control group vs. study group). The second independent variable (within subject factor) was measuring periods with 2 levels (beforetreatment vs. after-treatment).
- Bonferroni correction test (Post hoc-tests) to compare between pairwise within and between groups of the tested dependent variables which P-value was significant from MANOVA test.
- Pearson simple correlation coefficient (Bivariate correlation) was performed to compute the relations and directions between weight with pain and muscle strength in both groups.
- Significant level: all statistical analyses were significant at 0.05 level of probability (P≤0.05).
Results
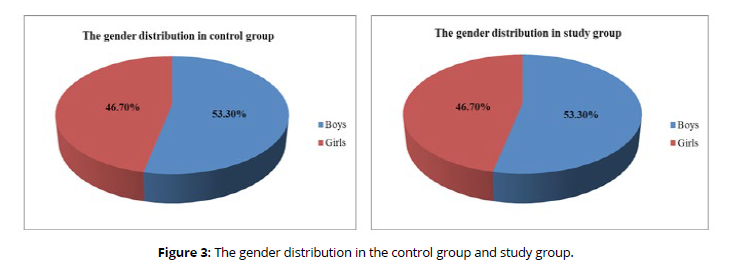
(Tables 5-10, figure 3)
| Items | Children general characteristics | |
|---|---|---|
| Age (Year) | BMI (kg/m2) | |
| Control group (n=15) | 9.33 ± 1.04 | 34.51 ± 2.62 |
| Study group (n=15) | 9.07 ± 0.96 | 34.06 ± 2.29 |
| t-value | 0.727 | 0.504 |
| P-value | 0.473 | 0.618 |
| Significance | NS | NS |
| Data are expressed as mean ± standard deviation (SD); P-value: probability value; NS: non-significant. This table shows that there was no significant difference in the mean values of children's ages (P>0.05) between the study group and the control group (P= 0.473) and BMI (P= 0.618). |
||
| Items | Gender | |
|---|---|---|
| Boys | Girls | |
| Control group (n=15) | 8 (53.3%) | 7 (46.7%) |
| Study group (n=15) | 8 (53.3%) | 7 (46.7%) |
| Chi-square value | 0.000 | |
| P-value | 1.000 | |
| P<0.05 | NS | |
| Data are expressed as number (percentage); P-value: probability value; NS: non-significant. This table shows no significant differences (P>0.05) in mean values of gender distribution (P=1.000) between the control group and study group. |
||
| Macronutrients | Before-treatment | Treatment (For all children) |
|
|---|---|---|---|
| Control group (n=15) | Study group (n=15) | ||
| Protein (%) | 15.56 ± 3.98 | 15.12 ± 5.68 | 30% |
| Fat (%) | 22.40 ± 10.67 | 35.82 ± 11.13 | 20% |
| Carbohydrates (%) | 57.48 ± 12.20 | 45.01 ± 15.50 | 50% |
| Total calories (kcal/day) | 3647.85 ± 950.22 | 3183.77 ± 879.39 | 2000 kcal/day |
| Data are expressed as mean ± standard deviation (SD). This table shows the difference between macronutrient intake before and during treatment program. |
|||
| Muscle group (Mean ±SD) | Control group | Study group | ||
|---|---|---|---|---|
| Before-treatment | After-treatment | Before-treatment | After-treatment | |
| Knee extensors | 6.52 ± 1.31 | 6.36 ± 1.38 | 6.74 ± 1.46 | 9.64 ± 2.00 |
| Knee flexors | 4.24 ± 0.97 | 4.16 ± 1.04 | 4.32 ± 0.98 | 6.06 ± 1.10 |
| Hip adductors | 4.10 ± 0.94 | 3.97 ± 1.04 | 4.20 ± 0.96 | 5.14 ± 0.71 |
| Hip abductors | 4.70 ± 1.24 | 4.54 ± 1.31 | 4.78 ± 1.00 | 6.48 ± 0.99 |
| Hip extensors | 6.24 ± 1.28 | 6.15 ± 1.34 | 6.19 ± 1.28 | 7.72 ± 1.32 |
| Hip flexors | 5.62 ± 1.10 | 5.46 ± 1.17 | 5.82 ± 1.21 | 6.78 ± 0.89 |
| Data are expressed as mean ± standard deviation. | ||||
| Muscle group | P value | Significance | ||
|---|---|---|---|---|
| Control group | Study group | Control group | Study group | |
| Knee extensors | 0.780 | 0.0001* | NS | S |
| Knee flexors | 0.846 | 0.0001* | NS | S |
| Hip adductors | 0.709 | 0.007* | NS | S |
| Hip abductors | 0.716 | 0.0001* | NS | S |
| Hip extensors | 0.846 | 0.002* | NS | S |
| Hip flexors | 0.681 | 0.021* | NS | S |
| P-value: probability value; S: significant;*: Significant (P<0.05); NS: non-significant. This table shows that in control group there was no significant difference in muscle power between before- and after-treatment while in study group, there was significantly increased muscle power after-treatment compared to before-treatment. Study group improved higher muscle power than control group. |
||||
| VAS (Mean ±SD) | |||
|---|---|---|---|
| Items | Control group (n=15) | Study group (n=15) | |
| Before-treatment | 5.13 ± 0.83 | 5.67 ± 0.97 | |
| After-treatment | 2.40 ± 0.18 | 1.20 ± 0.08 | |
| Mixed MANOVA (Overall effect) | |||
| MANOVA Overall effect | F-value | P-value | Significance |
| Group effect | 6.806 | 0.021* | S |
| Time effect | 184.307 | 0.0001* | S |
| Interaction (Group x Time) effect | 10.682 | 0.002* | S |
| Comparison between before- and after-treatment within each group (time effect) | |||
| Time effect | Control group (n=15) | Study group (n=15) | |
| Mean difference (change) | 2.73 | 4.47 | |
| Improvement % | 53.22% | 78.84% | |
| 95% CI | 1.98 – 3.48 | 3.71 – 5.21 | |
| F-value | 53.124 | 141.865 | |
| P-value | 0.0001* | 0.0001* | |
| Significance | S | S | |
| Comparison between both groups at before- and after-treatment (group effect) | |||
| Group effect | Before-treatment | After-treatment | |
| MD (change) | 0.54 | 1.20 | |
| 95% CI | -0.21 – 1.28 | 0.45 – 1.95 | |
| F-value | 2.023 | 10.239 | |
| P-value | 0.161 | 0.002* | |
| Significance | NS | S | |
| Data are expressed as mean ± standard deviation; CI: confidence interval; P-value: probability value; S: significant;*: Significant (P<0.05); NS: non-significant This table shows significant difference (MD=1.20; P=0.002; P<0.05) in the mean ± SD values of VAS between control group and study group at after-treatment (2.40 ± 0.18 and 1.20 ± 0.08, respectively). So, the decrease in pain score at post-treatment is greater in the study group (1.20 ± 0.08) than control group (2.40 ± 0.18). |
|||
Discussion
The purpose of the this study was to investigate the effect of strengthening and neuromuscular training on lower limb muscle strength and musculoskeletal pain in obese children in order to clarify the significance of physiotherapy rehabilitation programs as a needed approach during weight loss in obese children with lower limb musculoskeletal symptoms.
The results of the study revealed that with a combined diet and rehabilitation program that focused on strength and neuromuscular exercise lasting six weeks in the study group versus diet only program in the control group,
• There was an improvement in lower limb pain in both groups as a result of weight loss. However, lower limb pain decreased significantly in the study group compared to the diet-only group.
• Muscle power had a significant improvement in the study group as a result of the training program while the diet-only group had no significant change in their muscle power.
There are several studies concerning the relationship between obesity and musculoskeletal problems but there is a lack of research concerning the management of the condition particularly a multidisciplinary one including the management of weight and musculoskeletal problems together so , our study focused on treating children with obesity as a whole to gain the best outcomes.
Our study findings supports that weight reduction alone can reduce the lower limb pain as it decreased in both the study and control group which underwent weight reduction only.
These findings were also reported by Riddle et al. who suggested that there is a dose-response link between body weight alterations and pain as well as function. Alterations in weight of less than 10% of body weight have the possibility of producing significant changes in function and pain (27).
This supports the fact that weight reduction alone can produce improvement in pain/discomfort in the lower limbs of obese individuals as a result of unloading the joint structures, reduced effect of obesity-induced inflammatory cytokines as well as improved psychological status which reduces the fear of movement.
However, more improvement in pain symptoms was found in the study group as a result of their adherence to a six-week quadriceps and hip muscle strength program in addition to neuromuscular exercises which was primarily concerned with facilitating a controlled lower-extremity alignment throughout single loading phase. For example, single limb support in walking stair climbing. These results corroborate the findings of a great deal of the previous work of Holm et al who found that strength training in addition to neuromuscular exercise and education had a greater effect on pain sensitivity and pain intensity in the obese group than neuromuscular exercise and education alone (28).
The effect of strength training in improving pain/ discomfort was explained by Jenkinsen, who stated that strength training enhances correcting muscle weakness deficiencies and knee instability causing pain reduction and enabling the affected person to perform more activity with less discomfort (29), in addition to the reduced effect of inflammatory cytokine levels as IL-6 which accompany exercise training as reported by capuron et al (30).
This finding may be related to strength training's capability to alter the biomechanical gait patterns, allowing the subject to walk during weight bearing with slighter pelvic contralateral drop and hip adduction. According to Horsak et al with more muscle control, participants are better able to prevent a medial knee stress during weight acceptance, control their pelvic motion more effectively from the front, and keep the pelvis and femur correctly positioned during the weight loading phase of locomotion, which unloads the joints and makes movement more comfortable (31).
This finding is supported by the findings of Messier et al who found both exercise and dietary management reduce pain intensity, levels of inflammatory cytokines such IL-6, and body weight more than either treatment by itself (32).
Our findings are consistent with those of Paans et al who found that after 8 months of adherence to an exercise program that included weight loss along with aerobic and strength training lower limb pain decreased in obese patients by 25%. This significant reduction in pain may be the result of the prolonged training time, which suggests that lengthening the training period will result in greater improvement (33).
This finding emphasizes the remarkable effect of strength training as an approach that can be added to future obesity management programs for children who suffer lower limb musculoskeletal symptoms to gain the best improvement.
Pain improvement can also be attributed to the neuromuscular exercise program which aimed mainly at regaining joint stability and improving balance facilitating the healthy patterns of movement which have been inhibited by pain and sedentary behavior.
This also accords with earlier observations of Ageberg and Roos who suggested that although it targets sensorimotor deficits and functional instability more directly than standard strength or aerobic training, neuromuscular exercise is possible and effective in alleviating discomfort symptoms and enhancing physical function (34).
Guzmán et al also noted that children with excess body weight have better static and dynamic posture stability after four weeks of neuromuscular training. From this perspective, it can be argued that physical rehabilitation programs for this demographic should include neuromuscular training (35).
However, these outcomes are contrary to that of Horsak et al who reported that a training program that included both strength training and neuromuscular exercise for obese teenagers had no effect on lower limb discomfort. However, only healthy adults were included in his sample. Therefore, baseline joint health was almost equivalent to that of a person of normal weight. Additionally, over the course of the 12 weeks, reported adherence was only about 57%, which is a very low percentage (31).
Increased knee valgus angles, wider steps, and muscle dysfunctions are frequently seen in overweight adolescents and children. They run the danger of experiencing higher joint stress, pain, and discomfort as a result of their poor gait patterns and lower extremity misalignments (36).
Numerous studies examining weight loss in obesity are available. However, there are very few research studies looking at how strength and neuromuscular training might help alleviate these uncomfortable symptoms. Our goal was to evaluate a training program that combines strength and neuromuscular exercises for the lower extremities from pain, muscle strength, and quality of life perspective.
Our results state that the designed training program was capable of significantly improving muscle power in the study group while the diet-only group had no significant change in their muscle power this might be the primary reason why pain and discomfort significantly improved in the study group in comparison with the control group.
As a result, the strength training program might be an effective approach for counteracting the progressive development of the lower limb biomechanical abnormalities. However, Adherence was relatively poor, which emphasizes the need to create more appealing programs for this group.
However, this finding comes in contrast to Handrigan et al who reported that after The weight loss program alone, the increase in relative strength was 22% for obese subjects. However, their strength measurement was taken after 12-month weight loss program and for different age categories. Future research should follow up strength and pain measurements through longer periods of time and for different age categories (37).
These outcomes may potentially develop into effects that are more clinically relevant when adherence, intensity and duration are higher. Future research should take these important matters into account. If our findings point in the right direction, it may be proven that a hip and knee strength training program might help obese children achieve better results in terms of reducing musculoskeletal pain and discomfort and building stronger muscles.
From the previous findings It can be concluded that a strengthening and neuromuscular training program was effective in improving lower limb muscle strength and musculoskeletal pain in obese children. Therefore, it can be a valuable addition when managing children who suffer from obesity and lower limb pain to gain the best outcome
Conclusion
From the results obtained from the current study, there was a statistically significant difference after treatment between the control group and the study group in muscle power and pain which was favorable of the study group. The strengthening and neuromuscular exercise training program was effective in improving lower limb muscle power and musculoskeletal pain in obese children.
References
Aaseth J., Roer, G. E., Lien L., & Bjorklund G (2019). Is there a relationship between PTSD and complicated obesity? A review of the literature. Biomedicine & Pharmacotherapy. 117(10):348-256.
Calenzani, G., Santos, F. F., Wittmer, V. I., Freitas, G. K. F., & Paro, F. M (2017). Prevalence of musculoskeletal symptoms in obeses patientes candidates for bariatric sugery and its impact on health-related quality of life. Arch, Endocrinol Metab.61(4):319-325.
El-Shafie AM, Hogran HH, Mohamed Dphein AH.(2014). Prevalence of obesity in primary school children living in Alexandria governorate. Menouf Med J; 27:529–532.
Peltonen M, Lindroos AK, Torgerson JS (2003).Musculoskeletal pain in the obese: a comparison with a general population and long-term changes after conventional and surgical obesity treatment.Pain;104(3): 549–557.
de Sa´ Pinto AL, de Barros Holanda PM, Radu AS, Villares SMF, Lima FR.(2006). Musculoskeletal findings in obese children. J Paediatr Child Health; 42:341–344
Christensen R, Bartels EM, Astrup A, Bliddal H (2007).Effect of weight reduction in obese patients diagnosed with knee osteoarthritis: a systematic review and meta-analysis.Ann Rheum Dis;66: 433–439
MacFarlane GJ, de Silva V, Jones GT. (2011). The relationship between body mass index across the life course and knee pain in adulthood: results from the 1958 birth cohort study. Rheumatology; 50: 2251–2256.
SM Smith1,2, B Sumar1 and KA Dixon1 (2014). 'Musculoskeletal pain in overweight and obese children', International Journal of Obesity, 38(11-15)
Taylor ED, Theim KR, Mirch MC, Ghorbani S.(2006). Orthopedic complications of overweight in children and adolescents. Pediatrics; 117: 2167–2174.
Bell LM, Curran JA, Byrne S, Roby H, Suriano K, Jones TW, et al (2011). High incidence of obesity co-morbidities in young children: a cross-sectional study.J Paediatr Child Health.47:911–917.
Thivel, D., Ring-Dimitriou, S., Weghuber, D., Frelut, M. L., & O'Malley, G. (2016). Muscle strength and fitness in pediatric obesity: a systematic review from the European Childhood Obesity Group.Obesity Facts,9(1), 52-63.
D. J. Tomlinson . R. M. Erskine . C. I. Morse . K. Winwood . Gladys Onambe´le´-Pearson (2015). 'The impact of obesity on skeletal muscle strength and structure through adolescence to old age', Biogerontology , 17(), pp. 467-483.
-Slemenda C, Heilman DK, Brandt KD, Katz BP, Mazzuca SA, Braunstein EM, Byrd D (1998). Reduced quadriceps strength relative to body weight: a risk factor for knee osteoarthritis in women? Arthritis Rheum 41(11):1951–1959.
Visser M, Goodpaster BH, Kritchevsky SB, Newman AB, Nevitt M, Rubin SM, Simonsick EM, Harris TB (2005). Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol A 60(3):324–333
Tomlinson DJ, Erskine RM, Morse CI, Winwood K, OnambelePearson GL (2014). Combined effects of body composition and ageing on joint torque, muscle activation and cocontraction in sedentary women. Age 36(3):9652. doi:10.1007/s11357-014-9652-1 .
Syed IY, Davis BL.(2000). Obesity and osteoarthritis of the knee:hypotheses concerning the relationship between ground reaction forces and quadriceps fatigue in long-duration walking. Med Hypotheses; 54: 182–185.
Jozwiak M, Pietrzak S, Tobjasz F (1997). The epidemiology and clinical manifestations of hamstring muscle and plantar foot flexor shortening.Dev Med Child Neurol.;39(7):481-483.
Dufek JS, Bates BT.(1990). The evaluation and prediction of impact forces during landings. Med Sci Sports Exerc; 22: 370–377. PMID: 2381305
Mentiplay, B. F., Perraton, L. G., Bower, K. J., Adair, B., Pua, Y. H., Williams, G. P., ... & Clark, R. A. (2015). Assessment of lower limb muscle strength and power using hand-held and fixed dynamometry: a reliability and validity study.PloS one,10(10), e0140822.
Lim B, Hinman RS, Wrigley TV, Sharma L, Bennell KL. (2008). Does knee malalignment mediate the effects of quadriceps strengthening on knee adduction moment, pain, and function in medial knee osteoarthritis? Arandomized controlled trial. Arthritis Rheum.;59:943–51.
Kraemer WJ, Ratamess NA, Fry AC (2006). Strength testing: development and evaluation of methodology. In: Maud PJ, Foster C, editors. Physiological Assessment of Human Fitness. Champaign, IL: Human Kinetics;p. 119–50.
Buckley TA, Hass CJ.(2012). Reliability in one-repetition maximum performance in people with Parkinson's disease. Parkinsons Dis.;2012:928736.
Levinger I, Goodman C, Hare DL, et al (2009). The reliability of the 1RM strength test for untrained middle-aged individuals. J Sci Med Sport.;12(2):310–6.
Wakahara T, Miyamoto N, Sugisaki N, Murata K, Kanehisa H,
Kawakami Y, Fukunaga T, Yanai T (2012). Association between regional differences in muscle activation in one session of resistance exercise and in muscle hypertrophy after resistance training. Eur J Appl Physiol 112:1569–157
Kawakami Y, Abe T, Kuno SY, Fukunaga T (1995) .Training-induced changes in muscle architecture and specific tension. Eur J Appl Physiol Occup Physiol 72:37–43
Bennell KL, Egerton T, Wrigley TV, Hodges PW, Hunt M, Roos EM, et al (2011). Comparison of neuromuscular and quadriceps strengthening exercise in the treatment of varus malaligned knees with medial knee osteoarthritis: a randomised controlled trial protocol. BMC Musculoskelet Disord.;12:276
Riddle, D. L., & Stratford, P. W. (2013). Body weight changes and corresponding changes in pain and function in persons with symptomatic knee osteoarthritis: a cohort study.Arthritis care & research,65(1), 15-22.
Holm, P. M., Petersen, K. K., Wernbom, M., Schrøder, H. M., Arendt‐Nielsen, L., & Skou, S. T. (2021). Strength training in addition to neuromuscular exercise and education in individuals with knee osteoarthritis—The effects on pain and sensitization.European Journal of Pain,25(9), 1898-1911.conventional and surgical obesity treatment.Pain;104(3): 549–557.
JenkinsonC M,DohertyM,AveryA J,ReadA,TaylorM A,SachT Het al.(2009).Effects of dietary intervention and quadriceps strengthening exercises on pain and function in overweight people with knee pain: randomised controlled trialBMJ;339:b3170doi:10.1136/bmj.b3170
Capuron, L., Poitou, C., Machaux-Tholliez, D., Frochot, V., Bouillot, J. L., Basdevant, A., Layé, S., & Clément, K. (2011). Relationship between adiposity, emotional status and eating behaviour in obese women: role of inflammation.Psychological medicine,41(7), 1517–1528. https://doi.org/10.1017/S0033291710001984
Horsak, B., Schwab, C., Baca, A., Greber-Platzer, S., Kreissl, A., Nehrer, S., ... & Wondrasch, B. (2019). Effects of a lower extremity exercise program on gait biomechanics and clinical outcomes in children and adolescents with obesity: A randomized controlled trial.Gait & posture,70, 122-129.
Messier, S. P., Mihalko, S. L., Legault, C., Miller, G. D., Nicklas, B. J., DeVita, P., ... & Loeser, R. F. (2013). Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial.Jama,310(12), 1263-1273.
Paans, N., van den Akker-Scheek, I., Dilling, R. G., Bos, M., Van Der Meer, K., Bulstra, S. K., & Stevens, M. (2013). Effect of exercise and weight loss in people who have hip osteoarthritis and are overweight or obese: a prospective cohort study.Physical therapy,93(2), 137-146.
Ageberg, E., & Roos, E. M. (2015). Neuromuscular exercise as treatment of degenerative knee disease.Exercise and sport sciences reviews,43(1), 14-22.
Guzmán-Muñoz, E., Sazo-Rodriguez, S., Concha-Cisternas, Y., Valdés-Badilla, P., Lira-Cea, C., Silva-Moya, G., ... & Méndez-Rebolledo, G. (2020). Four weeks of neuromuscular training improve static and dynamic postural control in overweight and obese children: A randomized controlled trial.Journal of motor behavior,52(6), 761-769.
Gushue, D. L., Houck, J., & Lerner, A. L. (2005). Effects of childhood obesity on three-dimensional knee joint biomechanics during walking.Journal of Pediatric Orthopaedics,25(6), 763-768.
Handrigan, G., Hue, O., Simoneau, M., Corbeil, P., Marceau, P., Marceau, S., ... & Teasdale, N. (2010). Weight loss and muscular strength affect static balance control.International Journal of Obesity,34(5), 936-942.