Research Article - (2024) Volume 19, Issue 1
Whole Body Vibration Versus Functional Strength Training On Balance In Children With Hemiparetic Cerebral Palsy A Random
Amany I. Sabra1*, Abdelaziz Ali Sherief2, Osama A El-Agamy3 and Sara Y. Elsebahy4*Correspondence: Amany I. Sabra, Resident of Physical Therapy, Menyet El-Nasr Central Hospital, Dakahlia Governorate, Egypt, Email:
2Professor of Pediatric, Faculty of Physical Therapy, Kafr El Sheikh University, Kafr El Sheikh, Egypt
3Professor and Head Pediatrics, Faculty of Medicine, Kafr El Sheikh University, Kafr El Sheikh, Egypt
4Lecturer of Pediatric, Faculty of Physical Therapy, Kafr El Sheikh University, Kafr El Sheikh, Egypt
Received: 10-Feb-2024 Published: 24-Feb-2024
Abstract
Background: Hemiparetic cerebral-palsy (CP) is a condition characterized by muscle weakness or paralysis on one side of the body.
Purpose: To compare the short- and immediate effects of functional-strength-training (FST) and Whole-bodyvibration (WBV) on children with hemiparetic cerebral palsy's balance
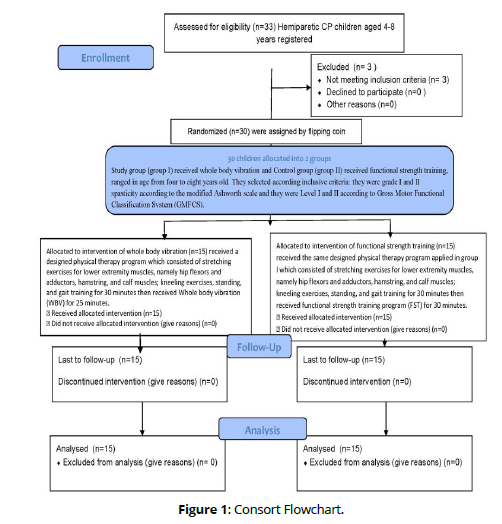
Methods: This Randomized Clinical Trial included Thirty-children split into two groups. Group A (n= 15) had Received 25-minute whole body vibration training session at a frequency of 20 to 30 Hz and an amplitude of 2 mm. Group B (n= 15) underwent gait training and functional strength training for 30-minutes.
Results: There was a noteworthy variation in both groups' gross motor function measure and biodex balancing system performance after treatment compared to pretreatment (P < 0.01). The Gross motor function measure of both groups demonstrated a significant difference (P < 0.01) between pretreatment and posttreatment in favor of group A. Similarly, the performance of the biodex balance system of both groups demonstrated a substantial variation (P < 0.01) pretreatment and posttreatment in favor of group A.
Conclusion: During a brief training period, whole body vibration has the potential to be more beneficial than functional strength workouts for improving the balance and gross motor functioning of children with hemiparetic CP.
Keywords
Hemiparesis. Cerebral palsy. Balance. Whole body vibration and Functional strength training
Introduction
The fundamental pathophysiology of cerebral palsy (CP) involves damage to the developing brain throughout the prenatal to neonatal period. It is predominantly a neuromotor disorder which impedes posture, tone of muscles, and movements. Even when the original neuropathological lesion is not progressing, children with CP might experience various types of secondary disorders over time that will differ in their impact on their functional capabilities [1].
Right or left arm and leg are typically affected by hemiparetic CP. and It can be identified by unilateral weakness or paralysis in muscles; Asymmetric impairment of muscular tone, balance, coordination, and posture is frequently the result of this disorder; Improving the affected person's spasticity and balance is the main goal of treatment for hemiparetic cerebral palsy; Numerous therapeutic approaches have been employed, such as extracorporeal shock wave therapy, dynamic ankle-foot orthoses, anticipatory posture modifications, and botulinum toxin injection. Whole-body vibration has surfaced as a promising therapeutic approach for hemiparetic cerebral palsy patients seeking to improve their balance [2].
Hemiparetic cerebral palsy children have impaired ankle control, which reduces the body's transverse rotation for postural stability Additionally, their motor activity is delayed., abnormal movement strategy timing, biomechanical restrictions, and compromised cognitive processing, and a reduced sense of verticality, all of which exacerbate balance issues [3].
Balance is a vital skill for persons with CP, since it helps them to conduct everyday activities such as walking, running, and playing; Functional strength training (FST) with whole-body vibration (WBV) are two therapies that have been demonstrated to enhance balance in children with hemiparetic CP [4].
WBV is a type of exercise where vibration is used to stimulate the nervous system and muscles, which can help to improve balance. This type of intervention is administered through a foot plate and is intended to stimulate the sole's somatosensory perception to promote brain plasticity. It has been demonstrated that whole-body vibration is useful for enhancing muscular endurance and balance control [5].
The goal of FST training is to build stronger muscles that are utilized in daily life. Children with CP may find it simpler to control their movements as a result, which may help to improve balance [6].
Our study's goal was to contrast the impact of FST and the impact of WBV has impacted on the balance and gross motor skills of children with hemiparetic CP.
Materials and Methods
A Randomized Controlled Trial had been used for the investigation. The Kafr Elsheikh University Faculty of Physical Therapy Outpatient Clinics served as the study's location. The study lasted from July 2023 to October 2023.
Participants
Using the G*POWER statistical program (version 3.1.9.2; Franz Faul, University at Kiel, Kiel, Germany), the sample size was determined. For this work, a minimum of thirty children would provide an appropriate sample size: one-tailed and a two-tailed test, a specification of Cohen’s (1988) effect size measure (d) under H1, the significance level α, the required power (1- β) of the test, and the preferred group size allocation ratio n2/n1 [7].
The subjects had been assigned into two groups at random by simple computerized randomization. Classified into two groups according to the criteria that follows: they required to be between the ages of four and eight; they had to be classified as having Spasticity Grade I and II on the Modified Ashworth Scale; they had to be at level I or II on the Gross Motor Functional Classification System (GMFCS); and they required the ability to comprehend simple instructions and follow orders. Any visual or auditory issues, uncontrollably shaking, fixed contractures and deformities, surgical intervention within the previous year, BOTOX injections into the calf muscle within the previous year, or a history of epileptic seizures disqualified the participants.
The work had been permitted by the ethics committee, Faculty of Physical Therapy, Kafrelsheik university (date of approval February 2023 with Number P.T/PED /2/2023/33), and number NCT05936554 clinical trials Protocol Registration and results system with Date of registration: July 6, 2023
For Evaluation
Every child has measured height and weight and document child data then assessed and selected according to inclusive criteria.
Modified Ashworth scale (MAS):
The MAS is utilized to quantify the extent of spasticity in both paediatric and adult populations exhibiting upper motor neuron diseases that was introduced by Bohannon and Smith [8].
Gross Motor Function Classification System Expanded and Revised (GMFCS-ER):
An objective way to track the evolution of gross motor function in children with CP is to use the Gross Motor Function Measure (GMFM), a standardized observational tool. Rather than evaluating the caliber of the child's motor performance, which evaluates how well the child completed the job, the GMFM evaluated motor function, or how much of a task the child could complete. It was created by Rasch Analysis and is the more recent version, GMFM-88 [9].
Biodex stability system:
Biodex Balance System is a valuable tool for research on balance. It is a comprehensive, objective, and reliable device that can be used to assess balance in people of all ages and abilities, and to track changes in balance over time. The device used in this study is sens balance Miniboard from Sensamove Company. Biodex Balance System is a valuable tool for research on balance. It is a comprehensive, objective, and reliable device that can be used to assess balance in people of all ages and abilities, and to track changes in balance over time [10].
With their hands on the handrails, every child had been instructed to position themselves in the center of the secured platform within the apparatus. The positioning of the display screen ensured that each participant had a straight line of sight to it. The gadget was first given the following parameters:
Child’s name, age, height, and weight. • Stability level (platform firmness).
Interventions
Preparation
Measuring height and weight and document child data then they were divided into two groups at random after providing their informed consent.
Test sessions time 1 minute, Then the child asked to be stable at same point for 1 minute, he tried to keep balanced and stable, lean on that his deviations score measured.
Treatment
Designed physical therapy program was given to children in both groups; It included kneeling exercises, standing and gait training as a warm-up for thirty minutes, and stretching activities for the lower extremity muscles, including the hamstrings, calf, and hip flexors and adductors. In group A to concentrate the vibration's energy on the lower extremities, the youngster stands on the WBV platform in a semi-squat posture (30 degrees of knee flexion). With frequency is between 20 and 30 Hz, and the vertical displacement is between 2 and 4 mm, the WBV application protocol consists of 25-minute period of vibration followed by 5 minutes of rest intervals [11]. The objective of the WBV device is to raise the frequencies of vibration from 28 to 30 Hz and the peak-to-peak displacement to 2 mm (specifically for the middle toe on both feet) by gradually increasing the frequency by 0.8 or 1 Hz per three sessions of treatment until reaching the desired frequency of 30 Hz. The rate at which the frequency of WBV increases is determined by the child's capacity to tolerate the vibration and their level of comfort with the chosen setting. The usage of a WBV device is likely to result in larger musculoskeletal force as the frequency and amplitude of the vibrations are increased [12]. Additional activities were added as training progressed on WBV, such as throwing and catching balls, moving uphill and downward while holding a stick in both hands, and pulling tiny objects with power, such pens, or balls [13]. In group B (n=15) a 30-minute functional strength training session, consisting of one to three sets of 10 to 15 repetitions maximum, to improve lower extremity muscle strength. Training frequency was split between two groups 3 times every week throughout a 12-week period [14]. Weights, higher steps, a lower bench, a slower pace, lessening the child's support, and/or performing more customized sets one-on-one are examples of progression; however, these options are typically modified after two weeks [15]. The functional strength training program was created to enable the affected leg's weak muscles to provide the necessary power in graded tasks or sequences of activities. Most of the exercises involved bearing weight and tested the participant's ability to balance while standing [16].
Step-up in front by affected leg: Assume a standing position and place the afflicted leg on a step forward. The young person ascends the step by lifting their entire body and descends it again.
Weight bearing on the affected leg: This entails keeping your weight on the affected leg while raising and lowering the non-affected leg up and down a step. Step up the afflicted leg sideways: Standing with the affected leg put on a step beside this leg. The youngster lifts their body sideways, descends, and then rises back up.
Raising the affected leg up on a step: While maintaining your weight on the unaffected limb, raise the affected leg forward and backward on a step.
Standing to sitting to standing: Standing. The youngster sits down until their buttocks touch the bench behind them, at which point they stand back up.
keeping both feet planted on the ground. stepping up and down on your toes Toes lift: when seated: Affected ankle's dorsal flexion when standing as advanced (like a heel walk): keeping both feet planted on the ground. Back on your heels and down once again
Bridging: Lying supine while flexing your knees and hips. Pelvis raising and lowering with feet on the bench, progress.
Results
Data analysis:
The Shapiro-Wilk test was conducted to assess the normality of the data. A chisquared test was utilized for contrasting the gender distribution among groups. Absolute descriptive statistics were used (The arithmetic mean is a statistical measure that describes the central tendency of a set of findings, while the standard deviation is a measure of how dispersed out the results are from the mean). Mann-Whitney tests were conducted for comparison of non-normally distributed scale variables between groups (pretreatment age, weight, height, and post treatment measurements of gross motor function measure and biodex balance system performance). Independent t test had been employed to contrast normally distributed scale variables between groups (pretreatment gross motor function measure and biodex balance system). Paired t test had been employed to contrast normally distributed scale variables within each group (between pretreatment and post-treatment measures of gross motor function), while wilcoxon test had been employed to contrast non normally distributed scale variables within each group (between pretreatment and post-treatment measures of biodex balance system performance). Level of significance for all statistical tests was set at P. value < 0.05 [17].
Between group comparison:
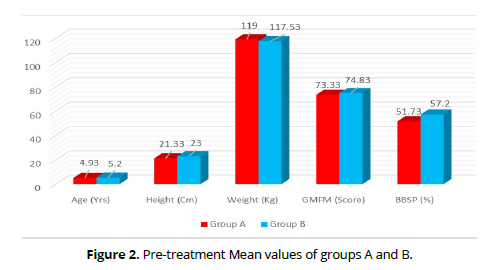
Preceding the therapy, no substantial variation was exited in age, weight, height, gross motor function measure and biodex balance system performance among both groups with P. value of (0.443, 219, 0.589, 0.156 and 0.14 respectively (Tables 1&2) (Figures 1&2), while after treatment, a substantial distinct gross motor function measure and biodex balance system performance among both groups in favour of group A with P. value of < 0.001 (Table 2).
| Gender | Group A | Group B | χ2 value | P. value | Sig |
|---|---|---|---|---|---|
| Female | 7 (46.7) % | 9 (60) % | 0.54 | 0.464 | NS |
| Male | 8 (53.3) % | 6 (40) % |
Dependent variables |
Group (A) (n = 15) |
Group (B) (n = 15) |
Group A Vs. B P. value* |
|
|---|---|---|---|---|
| Age | 4.93±1.16 | 5.2±1.08 | 0.443NS | |
| Weight | 21.33±2.61 | 23±4.16 | 0.219NS | |
| Height | 119±10.45 | 117.53±10.18 | 0.589NS | |
| Gross motor function measure |
Pre treatment | 73.33±2.34 | 74.83±3.21 | 0.156NS |
| Post treatment | 84.39±1.72 | 76.96±1.76 | < 0.001S | |
| % of change | 15.08 % | 2.85 % | ||
| P. value** | < 0.001S | 0.001S | ||
| Biodex balance system performance |
Pre treatment | 51.73±8.76 | 57.2±10.84 | 0.14NS |
| Post treatment | 87.92±5.7 | 67.47±6.13 | < 0.001S | |
| % of change | 69.96 % | 17.95% | ||
| P. value** | < 0.001S | 0.001S | ||
Within group comparison:
Regarding Goss motor function measure, both groups showed a significant difference (P < 0.01) posttreatment as compared with pretreatment in favor of group A with percent of change 15.08% & 2.85% respectively, while regarding biodex balance system performance both groups showed a significant difference (P < 0.01) posttreatment as compared with pretreatment in favor of group A with percent of change 69.96% & 17.95% respectively (Table, 2). Improvements can be detected by negative mean difference scores (95% confidence interval [CI]) on outcome measures.
Discussion
Whole-body vibration triggers the tonic vibration reflex, which sets off oscillatory vibrations that eventually lead to changes in muscle length. Primary sensory receptors in the affected muscle spindles are stimulated as a result, increasing the number of reflexive contractions [18]. WBV treatment improves muscle power and strength, which has a good impact on muscle performance as well as quick improvements in neuromuscular capacity [4]. The individual is placed in a standing position while receiving WBV therapy on an oscillating platform that vibrates horizontally between 10 and 25 Hz. This contributes to the stimulation of motor neuron activity and the main terminals of muscle spindles; this subsequently leads to contractions of the muscles and the tonic vibration reflex. Low frequency therapy results in a reduction in muscle tone as opposed to high frequency 40Hz, which promotes muscle tone. Therefore, WBV therapy enhances inter-muscular and intra-muscular coordination by stimulating high-frequency contractions of muscle in both the agonist and antagonist muscles of the neuro-muscular system. WBV therapy produces a stretch reflex that is useful for enhancing muscular endurance and balance control. This primarily increases the power in people who have motor limitations [19].
WBV improved the range of motion in the ankle joint and improved gross motor function in children with CP affecting the lower extremities, according to a meta-analysis by Xiaoye Cai and colleagues. WBVT has been shown to reduce timed up and go test scores, which lowers the risk of falling. They concluded that, in terms of enhancing the motor skills of the lower limb of children with CP, whole-body vibration therapy exceeds conventional kinds of physiotherapy in effectiveness [13].
Previous studies have highlighted how crucial it is to preserve muscle strength in the affected leg to enable a functioning gait in children who are hemiparetic. To address this problem, WBV has been apparent as a prospective intervention that can improve muscular force and mobility. High frequency, low amplitude WBV has been shown in studies by adults and children to have positive effects on muscle force and mobility, making it an appealing addition to therapeutic intervention [20].
All the chosen studies came to the same overall conclusion: WBV was a novel, secure, and useful therapy approach. WBV was very recently presented as a cutting-edge method to help individuals with cerebral palsy with their posture, locomotion, motor abilities, muscle strength, proprioception, static and dynamic balance, and gross motor skills [21]. Previous studies in this field have looked at the viability, safety, and efficacy of home-based WBV therapy for the first time in cerebral palsy patients. Studies have shown that applying WBV in conjunction with passive muscular stretching can lessen stiffness and enhance strength of the muscle and balance control in children and adolescents with CP. For adolescents and children with CP doing both home therapy and clinical therapy programs, WBV may be a supplement to muscular stretching [11].
FST provides a beneficial impact on both strength of the muscles and its movement in children who suffer from spastic CP [22], Park, and Kim's publication [23], which included patients of all ages with cerebral palsy, discovered beneficial results for strength and gait in randomised clinical trials. Research on muscle strengthening programs for stroke patients typically indicates that these interventions enhance gait, muscle strength, function of muscles, control of postures, balance, quality of life, and independence without causing increased stiffness or activity. While looking through the literature on FST regimens for different neurological disorders, this information was found. Additionally, improvements in the lower and upper extremities have been recorded within this condition. However, additional study falls short of showing advantages in particular gait and balance areas [24].
The research conducted by Taylor et al. [25] investigated the effects of increasing resistance training on the ability to move effectively in 47 individuals with spastic CP (average age: 18 years) who were categorized as GMFCS levels II and III. Out of the total number, 23 individuals engaged in strength training two times per week for a period of 12 weeks, utilizing a leg press. The researchers noticed a 27% improvement in the strength of the muscles (95% CI: 8-46) and a 14.8 kg rise in leg press maximum (95% CI: 4.3-25.3) in the therapy group. Additionally, there was a 0.8 unit rise in the functional mobility scale (95% CI: 0.1-1.6, P =.02). Nevertheless, no significant variations were noted in the average disparities for the 6-minute walk test (0.1 m; 95% CI: −20.6 to −20.9), the 10-m walk test (mean difference, 0.01 m/s; 95% CI: −0.06 to 0.07), or the GMFM E score (mean difference, 0.9%, 95% CI: −3.0 to 4.7). In another research study, participants diagnosed with spastic unilateral and bilateral CP (with an average age of 10 years and classified as GMFCS levels I–II) underwent a 12-week program of progressive FST, which was conducted three times per week. Scholtes et al. [26] analyzed the outcomes of this intervention. Subjects engaged in functional exercises such as half knee raise, sit-to-stand, and lateral step-up while wearing a weighted backpack. Additionally, they performed one activity using the leg presses. There were no significant differences in the GMFM-66, sit-to-stand, or lateral step-up tests. However, they did observe an 8% enhancement in strength of the muscles, evaluated using a hand-held dynamometer, and a 14 percent rise in the maximum number of repetitions on the leg press. Peungsuwan et al. [27] found that individuals with hemiplegic or diplegic CP showed improved walking endurance, speed of walking, strength in the muscles of the leg, and physical balance following undergoing eight weeks of combination training.
In a work conducted by Vulpen et al. [28], patients with CP aged 4 to 10 years old (3 times a week for 60 minutes over 14 weeks) were asked to rate their ability to walk and their strength in the plantarflexor muscle. The program included high-velocity resistance exercises. After training, they demonstrated an 83% increase in muscle power during the sprint test.
FST has a beneficial impact on muscle strength and movement in children with spastic CP. However, there is limited information about the long-term consequences of FST [22].
By implementing strength programs specifically designed for children and adolescents with CP, researchers observed an improvement in both walking speed and overall motor skills, without any increase in spasticity of the muscles. The lower extremity muscle groups that are weak because of the neurological injury and subsequent decrease in activity have become stronger, according to these results, suggesting that the workload capacity and resistance of these muscles may be enhanced. Furthermore, there is an increase in walking speed, suggesting that kids and teenagers will be able to move more functionally. Additionally, there is an enhancement in gross motor function, or a person's capacity to carry out certain voluntary movements and tasks (like running or jumping). Ultimately, a significant improvement in balance was attained.
A strength training program can have beneficial impacts on the strength of the muscles, balance, gait speed, and gross motor function for children and adults with CP who are classified in levels I, II, and III of the GMFCS. These effects can be achieved without increasing spasticity if the program is administered with appropriate dosage and follows specific principles [29].
However, our findings contradict those of Scianni et al. [30], who found that strength training has no beneficial effects on any variables in the population of people with cerebral palsy.
WBV training is a straightforward and non-invasive method that is relatively safe and requires a short training time for individuals with CP. A single intervention may result in favorable outcomes, enhancing the motivation and enthusiasm for rehabilitation in children. The integration of WBV training with traditional treatment has the potential to enhance rehabilitation and yield superior treatment results [13]
Whole-body vibration therapy and functional strength training are two promising interventions that can help these children with their balance. These therapists can be included in treatment plans to help kids with hemiparetic cerebral palsy improve their postural control and balance, which will ultimately improve their motor function and quality of life [31].
Conclusion
To sum up, the research conducted on the impact of WBV and FST on balance in children diagnosed with hemiparetic CP yielded encouraging results, indicating that the combined intervention may improve balance in these children. Numerous studies have shown that WBV helps children with CP walk more easily, balance better, fall less frequently, have functional mobility, and have better gait function.
Recommendation: need further research to evaluate the impact of wholebody vibration on different variables and different disease
Further research endeavors that do a longitudinal quantitative and kinematic examination may yield more exhaustive data concerning the alterations in gait function that are linked to motor recovery.
Further studies should compare the benefits of functional strength training and whole-body vibration to other therapies, including treadmill training with partial body weight support, for enhancing balance and gait function in kids with hemiparetic cerebral palsy.
Acknowledgments: Nil
References
Furtado MAS, Ayupe KMA, Christovão IS, Sousa Junior RR, Rosenbaum P, Camargos ACR, et al. (2022) Physical therapy in children with cerebral palsy in Brazil: a scoping review. Developmental Medicine & Child Neurology 64:550-560.
Patel DR, Neelakantan M, Pandher K, Merrick J (2020) Cerebral palsy in children: a clinical overview. Translational Pediatrics 9:S125-s135.
Mishra S, Potdar R (2021) Effect of additional load on angular parameters during gait and balance in children with hemiparesis – Cross sectional study. Biomedical Human Kinetics 13:128-138.
Jung Y, Chung EJ, Chun HL, Lee BH (2020) Effects of whole-body vibration combined with action observation on gross motor function, balance, and gait in children with spastic cerebral palsy: a preliminary study. Journal of Exercise Rehabilitation 16:249-257.
Hegazy RG, Abdel-Aziem AA (2022) Effect of Whole-Body Vibration Exercise on Hamstrings-to-Quadriceps Ratio, Walking Performance, and Postural Control in Children With Hemiparetic Cerebral Palsy: A Randomized Controlled Trial. Journal of Manipulative & Physiological Therapeutics 45:660-670.
Rausch M, Weber F, Kühn S, Ledderhos C, Zinner C, Sperlich B (2021) The effects of 12 weeks of functional strength training on muscle strength, volume and activity upon exposure to elevated G(z) forces in high-performance aircraft personnel. Military Medical Research 8:15.
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods 39:175-191.
Bohannon RW, Smith MB (1987) Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther 67:206-207.
Palisano RJ, Rosenbaum P, Bartlett D, Livingston MH (2008) Content validity of the expanded and revised Gross Motor Function Classification System. Developmental Medicine & Child Neurology 50:744-750.
Cachupe WJC, Shifflett B, Kahanov L, Wughalter EH (2001) Reliability of Biodex Balance System Measures. Measurement in Physical Education and Exercise Science 5:97-108.
Han YG, Lee SW, Yun CK (2019) The immediate influence of various whole-body vibration frequency on balance and walking ability in children with cerebral palsy: a pilot study. Journal of Exercise Rehabilitation 15:597-602.
Liu P, Li Y, Xiao Y, Li D, Liu L, Ma Y, et al. (2023) Effects of whole-body vibration training with different frequencies on the balance ability of the older adults: a network meta-analysis. Frontiers in Physiology 14:1153163.
Cai X, Qian G, Cai S, Wang F, Da Y, Ossowski Z (2023) The effect of whole-body vibration on lower extremity function in children with cerebral palsy: A meta-analysis. PLoS One 18:e0282604.
Ahmed A, Asghar E, Iftikhar S, Hayat S, Hussain SA, Farooq N (2022) Effects Of Trunk Exercises On Balance Among Children With Cerebral Palsy. Multicultural Education 8.
Ahern L, Nicholson O, O'Sullivan D, McVeigh JG (2021) Effect of Functional Rehabilitation on Performance of the Star Excursion Balance Test Among Recreational Athletes With Chronic Ankle Instability: A Systematic Review. Archives of Rehabilitation Research and Clinical Translation 3:100133.
Abd-Elfattah HM, Ameen FH, Elkalla RA, Aly SM, Abd-Elrahman NAF (2022) Loaded Functional Strength Training versus Traditional Physical Therapy on Hip and Knee Extensors Strength and Function Walking Capacity in Children with Hemiplegic Cerebral Palsy: Randomized Comparative Study. Children (Basel) 9.
Zoubir A, Koivunen V, Ollila E, Muma M. Robust Statistics for Signal Processing2018.
Sedano Ibarra LJ (2022) The efficacy of whole-body vibration and balance training on dynamic balance and eversion strength in active adults with chronic ankle instability: a meta-analysis.
Lee W-B, Lee H-S, Park S-W, Yoo J-K (2019) Effects of whole body vibration training on lower limb muscle thickness and gross motor function in children with spastic cerebral palsy. Journal of the Korean Society of Physical Medicine 14:195-201.
Srisaphonphusitti L, Manimmanakorn N, Manimmanakorn A, Hamlin MJ (2022) Effects of whole body vibration exercise combined with weighted vest in older adults: a randomized controlled trial. BMC Geriatrics 22:911.
Hegazy RG, Abdel-aziem AA, El Hadidy EI, Ali YM (2021) Effects of whole-body vibration on quadriceps and hamstring muscle strength, endurance, and power in children with hemiparetic cerebral palsy: a randomized controlled study. Bulletin of Faculty of Physical Therapy 26:6.
Shilesh K, Karthikbabu S, Rao PT (2023) The Impact of Functional Strength Training on Muscle Strength and Mobility in Children with Spastic Cerebral Palsy - A Systematic Review and Meta-Analysis. Developmental Neurorehabilitation 26:262-277.
Park EY, Kim WH (2014) Meta-analysis of the effect of strengthening interventions in individuals with cerebral palsy. Research in Developmental Disabilities 35:239-249.
Tupimai T, Peungsuwan P, Prasertnoo J, Yamauchi J (2016) Effect of combining passive muscle stretching and whole body vibration on spasticity and physical performance of children and adolescents with cerebral palsy. The Journal of Physical Therapy Science 28:7-13.
Taylor NF, Dodd KJ, Baker RJ, Willoughby K, Thomason P, Graham HK (2013) Progressive resistance training and mobility-related function in young people with cerebral palsy: a randomized controlled trial. Developmental Medicine & Child Neurology 55:806-812.
Scholtes VA, Becher JG, Comuth A, Dekkers H, Van Dijk L, Dallmeijer AJ (2010) Effectiveness of functional progressive resistance exercise strength training on muscle strength and mobility in children with cerebral palsy: a randomized controlled trial. Developmental Medicine & Child Neurology 52:e107-113.
Peungsuwan P, Parasin P, Siritaratiwat W, Prasertnu J, Yamauchi J (2017) Effects of Combined Exercise Training on Functional Performance in Children With Cerebral Palsy: A Randomized-Controlled Study. Pediatric Physical Therapy 29:39-46.
van Vulpen LF, de Groot S, Rameckers E, Becher JG, Dallmeijer AJ (2017) Improved Walking Capacity and Muscle Strength After Functional Power-Training in Young Children With Cerebral Palsy. Neurorehabil Neural Repair 31:827-841.
Merino-Andrés J, García de Mateos-López A, Damiano DL, Sánchez-Sierra A (2022) Effect of muscle strength training in children and adolescents with spastic cerebral palsy: A systematic review and meta-analysis. Clinical Rehabilitation 36:4-14.
Scianni A, Butler JM, Ada L, Teixeira-Salmela LF (2009) Muscle strengthening is not effective in children and adolescents with cerebral palsy: a systematic review. Australian Journal of Physiotherapy 55:81-87.
Hassan Z, Rasanani MRH, Hussain SA, Shadmehr A, Talebian S, Bagheri H, et al. (2024) The Possibility of Improvement in Balance and Function Following Conjunct Effects of Transcranial Direct Current Stimulation and Whole-Body Vibration Therapy in Spastic Cerebral Palsy Patients: A Hypothesis Study. Journal of Health and Rehabilitation Research 4:447-455.