Research Article - (2023) Volume 18, Issue 6
Mulligan Mobilization Technique Versus Neural Mobilization On Nerve Root Function In Patients With Cervical Radiculopath
Rania N Karkousha1, Amany I Selem2*, Maher A El kablawy3, Samir A Aly4 and Magda R Zahran1*Correspondence: Amany I Selem, hysiotherapist, Ismailia Medical Complex, Egypt, Email:
2hysiotherapist, Ismailia Medical Complex, Egypt
3Professor, Department of Basic Sciences, Faculty of Physical Therapy, Cairo University, Egypt
4Lecturer, Department of Neurology, Faculty of Medicine, Suez University, Egypt
Received: 13-Dec-2023 Published: 25-Dec-2023
Abstract
Objective: To look into the impact of Mulligan mobilization versus neural mobilization on nerve root function.
Methods: Seventy-two cervical radiculopathy patients were randomly divided into three separate groups of equal size; group A was administered Mulligan therapy besides conventional treatment, group (B) was administered neural mobilization besides conventional treatment and group (C) was administered conventional treatment only, over the course of four weeks, treatment was administered to each group three times weekly. Electromyography device was utilized to measure peak to peak amplitude, latency and F-wave, while digital commander algometer was utilized to assess pressure pain threshold as well as Arabic version of Neck Disability Index was utilized to assess cervical neck function.
Results: In all measured variables, There was no statistically significant difference among three groups pretreatment as p>0.05, while was a statistically significant difference among the three groups post-treatment, with a p-value of less than 0.05. Group B showed more favorable results. Additionally, there was a statistically significant difference between the pre and post-treatment measurements in groups A and B for all variables, while there was only statistical substantial difference in pressure pain threshold as well as cervical neck function in group C as p<0.05.
Conclusion: Both Mulligan mobilization technique as well as neural mobilization have a positive effect on amplitude, latency, F-wave, pressure pain threshold and neck function with more superiority to neural mobilization. Both techniques are effective in the rehabilitation of patients with cervical radiculopathy.
Keywords
Cervical radiculopathy. Mulligan mobilization. Nerve root function. Neural mobilization
Introduction
Cervical radiculopathy (CR) is characterized by a radicular pain distribution in either or both of upper extremities, resulting from constriction as well as aggravation of more than one cervical nerve roots. Between 70% and 75% of individuals experience CR owing to the mixture of degenerative modifications, while 20% to 25% of cases are caused by disc herniation 1. It has an incidence rate between 0.83 and 1.79 per 1000 person per year these numbers are expected to increase due to the aging population 2. Cervical radiculopathy has an equal impact on both males and females in their forties and fifties 3, and it may be unilateral or bilateral 4. Individuals who have both neck pain and upper extremity symptoms tend to have higher levels of disability compared to those who only have neck pain. Additionally, the C7 nerve root is the most commonly impacted level, followed by the C6 nerve root 5.
Cervical radiculopathy results in pain and impairments that significantly diminish the individual's health-related quality of life 6. Mild symptoms of pain and numbness may be present, however in severe cases; cervical radiculopathy will be accompanied by motor weakness. Patients with CR also have myofascial trigger points in upper back musculatures including middle trapezius which may be associated with cervical nerve roots compression that activate the starting for either active or latent triggers points 7.
Several research papers have demonstrated the advantages of manual methods and physical therapy on individuals experiencing neck pain, regardless of whether they have radicular symptoms or not. This includes patients with cervical radiculopathy 8. Mulligan Techniques are novel manual therapy techniques used by physiotherapists for the management of CR 9. Sustained natural apophyseal glides (SNAGs) refer to a type of manual therapy that combines sustained facet glides with active physiological movement to reach the maximum range of motion, performed by the patient. Subsequently, painless passive end-of-range overpressure or stretching is applied as a barrier 10.
Neural mobilization (NM) is indicated as a manual therapy technique to alleviate pain and improve impairment in patients. It is also suggested as a treatment option for pain relief 11. NM refers to a set of methods that utilize a precise sequence of joint movements to mobilize the peripheral nerve involved, with the aim of improving nerve gliding and reducing neural mechanosensitivity 12.
According to literature, there were two previous studies reported the role of mulligan mobilization technique and neural mobilization on neck disability, pain as well as ROM among patients suffering from cervical radiculopathy 13. But those studies didn’t report the role of Mulligan mobilization technique and neural mobilization on nerve root function and F-wave in patients with CR so this study was conducted to compare between Mulligan mobilization technique and neural mobilization on nerve root function (peak to peak amplitude, latency), F-wave, pressure pain threshold (PPT) and neck function among patients suffering from CR.
Material and Methods
Study design
Randomized control trial with pre and post-test design was performed in the physiotherapy out clinic of Esmaellia hospital from March 2023 to July 2023. The study conducted by the Faculty of Physical Therapy at Cairo University in Egypt has been authorized by the Ethical Committee for Human Research (Approval No: REC/012/003994) and registered with Clinical Trials Registration (NCT05803954). Patients were invited to participate in this trial and completed the written consent form before taking part.
Sample size
G-Power software version 3.0.10 was used for computing sample size. The F-test for MANOVA was taken to examine the interaction effects within and between groups. Given a statistical power of 0.80, a significance threshold (α) of 0.05 (two-tailed) with effect size = 0.37, the sample size required for the study is 72 individuals, with 24 participants in each of the three groups.
Randomization
Through the use of computer-generated random block randomization with block sizes of three and six, 72 patients with CR were randomly assigned to three equal sizes groups. The concealed allocation was performed utilizing sealed opaque envelopes by the fifth author, who was not involved in the recruitment, data collection, or treatment of the subjects. The first author conducted measurements of all variables. Ultimately, the second author unsealed the envelopes and proceeded to provide treatment in accordance with the assigned groups.
Participants
A total of seventy-two cases, comprising individuals of both genders, were diagnosed with cervical radiculopathy by neurologist and referred to physiotherapy out clinic of Ismailia hospital. Patients in this experiment had to be between the ages of 20 and 50 years old to be eligible to enroll 13, although had cervical disc (C 5-C 6 and/or C 6- C7) herniation with both sensory and motor nerve affections, they also had neck pain that extended down to the arm. The Spurling test, Upper Limb Tension Test 1 (ULTT1), cervical distraction test, and cervical rotation test all yielded positive results, indicating symptoms were exacerbated during these assessments 13, BMI from 18 to 25 kg/m2 and Existed active trigger points within middle trapezius and/ or cervical region.
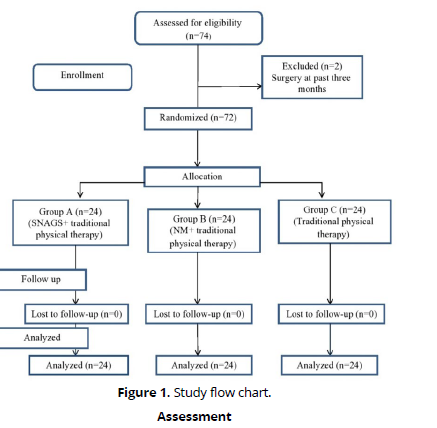
Patients who had cardiovascular or respiratory disorder, vertebra basilar insufficiency, osteophytes in cervical vertebra, spinal fracture or surgery, nerve lesion or received physical therapy treatment in the previous three month were excluded from the trial. (Figure 1) represents the flow chart of the study. Seventy four patients with CR were recruited from physiotherapy out clinic of Ismailia hospital. The inclusion criteria were not met by two patients since their treatment had been completed more than three months ago. Therefore, 72 patients met the inclusion criteria for the study.
Assessment
1-Nerve root function and F-wave
Peak to peak amplitude, nerve latency and F wave were measured using an electromyogram device (Neurosoft, Ivanova, Russia). Full relaxation of the patient must be obtained; on cushions beneath the legs and head and a gently padded table, the subject was laying supine. Methylated alcohol was used to clean the skin in preparation, drying the skin by rubbing it with dry clean cotton wool to diminish the skin resistance under both the stimulating electrode and recording electrodes.
After separating the hair and properly cleaning the skin in between by methylated alcohol, the skin areas were gently abraded using sand paper, which removed many superficial layers of skin and skin oils. Using this technique helped to overcome the skin impedance since, as is commonly believed, abrasion is adequate when the impedance measured between 1,000 as well as 5,000Ω across two such electrode preparation sites 14.
Stimulations
Using a square wave pulse with a constant current and a duration of 0.2 ms, transmitted at 3.1 Hz, stimulation was carried out. Using an examination time of 50 ms, the average cortical responses were magnified and displayed. Using 2 Hz to 1 KHz as a filters setting. The traces were then superimposed to guarantee reproducibility, and negative near field potentials were collected to quantify the peak to peak amplitude 15. In order to evaluate the dermatomes of C6 and C7, bipolar stimulating electrodes were put approximately 7 cm above the styloid process of the radius and between the second and third metacarpal bones. The electrode spacing between the electrodes was 2.5 cm 15.
Recording
To find every position required for DSSEPs, four common landmarks have to be found. The first pain of anatomical land mark present in the skull mid sagittal plane in the form of nasion (bridge of the nose) and inion (posterior bony protuberance over the inferior aspect of the occiput). The second pair of landmarks in the frontal plane are the areas immediately anterior to the tragus, which are the areas where the ears attach to the skull. An electrode site known as the CZ is located at the vertex of the skull, which is identified by the point at which the line connecting the two ears crosses the previously identified mid-point of the sagittal line connecting the nasion and inion. An electrode site known as FpZ is formed by 10% of the entire distance, superior to nasion, between the nasion and inion. The recording location is 20% of the entire distance from CZ toward the nasion and the inion, the two sites mentioned above. The reference electrode and ground electrode were positioned at Fz and Fpz points, respectively, while the recording electrodes were located at C3' and C4' (between C3 and P3 and C4 and P4) in the international electroencephalogram 10–20 system.
Measured variables
Positive peak and negative near field potential were identified to determine the peak-to-peak amplitude after the stimulation was carried out and the traces were merged to guarantee reproducibility. A peak's amplitude is the distance measured between its positive and negative peaks.
2. Pressure pain threshold
Pressure pain threshold was measured by a Commander-Algometer device (JTECH Medical Company; Midvale). To evaluate deep-tissue pain sensitivity, it uses physical pressure created by the device. Because of its validity and reliability, this device is often used for estimating pressure pain thresholds 16. In order to evaluate the subject's pressure pain threshold as well as upper trapezius muscle tenderness, the subject was asked to identify the pain. Following pincer palpation, the region was identified and marked. The power is turned on, and the transducer probe tip was applied over those areas perpendicularly. The transducer was firmly pressed downward to apply the necessary pressure on the points. The pressure at the point, expressed in pounds force, was shown on the digital display. The amount of pressure applied was maintained and increased gradually until the person complained of pain and said, "STOP." At this moment, the pressure pain threshold value was displayed digitally. Pressing the HOLD switch allowed this value to be stored 16.
3. Neck Function
The neck function was assessed by the Arabic version of Neck Disability Index questionnaire tool which has reliability and validity 17 .Ten sets are included, with six options in each (0–5) 18. 0–4 represents no disability; 5–15 denotes mild disability; 5–14 denotes moderate disability; 25–34 denotes severe disability; and >34 denotes total impairment. The option that most closely matched their function was asked of the patients to choose.
Outcome measures
All variables were measured twice, first one before starting and the second after four week of intervention. The primary outcome measures were nerve root function in the form of peak to peak amplitude and latency, F-wave and PPT. The secondary outcome was neck function.
Intervention
Group (A) were given SNAGS Mulligan mobilization technique besides conventional treatment, group (B) were given neural mobilization besides conventional treatment while group (C) were given conventional treatment only for four weeks, three times a week.
Group A: For rotation or side bending: On a stool, the patient was sitting in erect posture and the therapist was standing behind the patient with engaging the medial border of one thumb's distal phalanx on the articular pillar on the suspected site of lesion. The angle at which the thumb nail slopes is roughly 45 degrees (in the direction of the eyeball). This is further reinforced by the therapist's other thumb. This indicates that the therapist's thumb was on the cervical sixth articular pillar if the patient had a lesion at cervical C6-7. On the other hand, if you SNAG on the right, lay your right thumb on the right pillar and use your left to push up. When the left thumb's SNAG would be on the left pillar. To keep the neck from flexing, the therapist's additional fingers should be comfortably placed laterally on either side of the neck or upper anterolateral thorax. The patient was instructed to turn his head slowly in the painfully restricted direction while the facet was being maintained. The patient is asked to apply continuous overpressure for a few seconds at a 45-degree angle toward the eyeball as the therapist follows the patient's head rotation with his hands to ensure mobilization occurs with the movement 19-20.
For flexion or extension: The participant was positioned in an erect posture on a chair, while the researcher stood behind him. At the spinous processes, the medial border of the right thumb's distal phalanx was placed, while the back of the left thumb supported the right thumb. The glide was administered in a central manner, aligning the direction of the facet joint towards the eyeball. The individual was advised to maintain the glide while actively flexing or extending, and to apply additional pressure at the end of the range when the comparable sign disappears, before returning to the beginning position. The mobilizations were repeated six times as well the movements were reevaluated 20 .There are a total of 20 oscillations, occurring at a rate of two to three oscillations per second, lasting for one to two minutes 19.
Group B: The patient was received grade two of median nerve neural mobilization. The time of oscillation was two or three oscillation in a second for one to two minutes. The patient was positioned obliquely on the bed, with his head oriented towards the side of the bed. The scapula was elevated off the bed, with the examiner's right thigh pressing against the patient's left shoulder.
He is holding the patient's arm with his right hand and their wrist with their left for support. Given the crossed-arm starting position, the physiotherapist's hand position needed few changes during the procedure, making the method smoother and easier to control (Stage 1).
Carefully depressing the patient's shoulder girdle with his thigh, the tester then did 10° of shoulder abduction to make the arm clear and parallel to the bedside (Stage 2).
The examiner then continued by keeping the patient's shoulder girdle depression, extending their elbow, and pronating their forearm (Stage 3). Maintaining all of these motions, the examiner laterally rotated the patient's whole arm with both arms (Stage 4) While maintaining this position, the examiner's left forearm was rotated such that the palm faced downwards and moved downwards towards the patient's hand. The examiner's thumb was then inserted into the space between the patient's thumb and index fingers. This position offers excellent dexterity and fine motor control across the entire arm, including the fingertips (Stage 5), finally the shoulder abduction was added (Stage 6) 21-22.
Group C (control group): The patients were given conventional therapy in the form of form of infrared radiation and ultrasound therapy.
Infrared application: Body LED Red Light Therapy Infrared light therapy lamp with a stand that may be adjusted. The 660nm Red-light as well as 850nm Infrared Light Device was applied for 10 minutes while the patient was lying face down. The device was positioned at a distance of 50 to 75 cm, depending on the patient's tolerance 15.
Ultrasound therapy application: Sonopower Due device is a therapeutic US device manufactured by life medical, serial number: LHC 2000 and it was used to conduct this study. Sonopower Due has a digital screen for time and intensity. It allows either pulsed or continuous mode, the head surface is five cm2. The patients received ultrasound from prone lying for 10 minutes with 1.5 w/cm2 intensity and frequency 1 Mega Hertz 15.
Statistical Analysis
The results of the Shapiro-Wilk test, which was used to determine whether the data were normal, showed that every variable had a normal distribution. MANOVA was carried out to contrast the effect of time as well as treatment among groups, as well as the interaction between time as well as treatment. Multiple pairwise comparison by Post-hoc testing were conducted for subsequent multiple comparisons. Through the use of SPSS version 22 for Windows, statistical measurements were carried with significance level of (p < 0.05). To compare the groups according to sex and affected side, chi-squared tests were utilized. ANOVA was used to compare among groups in physical characteristics.
Results
ANOVA did not find any statistically substantial differences in any of the physical attributes across the three groups as presented in (Table 1).
| Group A | Group B | Group C | f-value | p-value | |
|---|---|---|---|---|---|
| Age (years) | 39 ± 4.6 | 38.8 ± 5.7 | 38 ± 5.2 | 0.24 | 0.79 |
| Weight (kg) | 66 ± 5.6 | 67.3 ± 8 | 68 ± 10 | 0.415 | 0.66 |
| Height (cm) | 166.7 ± 7.5 | 171.6 ± 9.5 | 172 ± 9.7 | 2.69 | 0.08 |
| BMI (kg/m 2) | 23.7 ± 1.6 | 22.8 ± 1.8 | 22.9 ± 1.9 | 1.76 | 0.18 |
| Genders | χ2=0.969 | 0.62 | |||
| (male/female) | 19 (79%) | 17 (70.8%) | 16 (66.7%) | ||
| 5 (21%) | 7 (29.2%) | 8 (33.3%) | |||
| Affected side | χ2=5.44 | 0.07 | |||
| Right | 16 (66.7%) | 8 (33.3%) | 13 (54%) | ||
| Left | 8 (33.3%) | 16 (66.7%) | 11 (46%) |
According to MANOVA results, there was statistical substantial difference among groups as groups as Wilks' Lambda (ʎ) = 0.25, F =12.76, p=0.0001 and ƞ2=0.49 also there was a substantial difference at a time as ʎ = 0.04, F =320.76, p=0.0001 as well as ƞ2=0.96. There was a significant interaction among group as well as time as ʎ = 0.16, F = 19.72, p=0.0001 and ƞ2=0.6.
Within and between group analysis: Multiple pairwise comparisons reported statistical substantial difference among pre as well as post-treatment in all variable at group A and B as p-value <0.05 (Table 2). In group C; there was statistical substantial in PPT and ANDI but there was no statistical substantial difference in peak to peak amplitude, latency and F-wave (Table 2). Among three groups analysis at pre-treatment revealed no statistical difference as p-value >0.05(Table 2) nevertheless, three groups showed statistically different results post-treatment. (Table 2) The results also reported in Table 3, there was statistical difference between A and C, and between B and C in all measured variables. Between A and B there was no statistical difference in peak to peak amplitude, latency, F-wave and ANDI but there was statistical difference in PPT (Table 3).
| Variables | Group A | Group B | Group C | p-value between |
f-value between |
Ƞ2 |
|---|---|---|---|---|---|---|
| Peak to peak amplitude (µv) | ||||||
| Pre-treatment | 1.66±0.23 | 1.64±0.28 | 1.61±0.29 | 0.76** | 0.28 | |
| Post-treatment | 2.26±0.31 | 2.33±0.28 | 1.66±0.27 | 0.0001 * | 19.32 | 0.54 |
| p-value (within) | 0.0001 * | 0.0001 * | 0.54** | |||
| MD | -0.59 | -0.69 | -0.047 | |||
| Latency (ms) | ||||||
| Pre-treatment | 20.53 ± 0.59 | 20.6 ± 0.6 | 20.6 ± 0.45 | 0.84** | 0.02 | |
| Post-treatment | 19.7 ± 0.33 | 19.4 ± 0.32 | 20.2 ± 0.24 | 0.0001 * | 44.8 | 0.56 |
| p-value | 0.0001 * | 0.0001 * | 0.06** | |||
| MD | 0.85 | 1.19 | 0.31 | |||
| F-wave | ||||||
| Pre-treatment | 26.96 ± 1.63 | 26.3 ± 5.47 | 26.7 ± 1.3 | 0.79** | 0.2 | |
| Post-treatment | 25.33± 0.7 | 24.94 ± 1.64 | 26.45 ± 1.21 | 0.0001 * | 9.46 | 0.21 |
| p-value (within-group) | 0.02* | 0.04* | 0.71* | |||
| MD | 1.63 | 1.37 | 0.25 | |||
| PPT (kg/cm2) | ||||||
| Pre-treatment | 0.71±0.28 | 0.72±0.21 | 0.7±0.18 | 0.98** | 0.02 | 0.03 |
| Post-treatment | 1.82±0.3 | 2.36±0.38 | 1±0.17 | 0.0001 * | 127.4 | 0.79 |
| p-value | 0.0001 * | 0.0001* | 0.0001 * | |||
| MD | -1.1 | -1.64 | -0.3 | |||
| ANDI | ||||||
| Pre-treatment | 25.95±3.5 | 26.33±2.52 | 27±4.95 | 0.85** | 0.16 | |
| Post-treatment | 12.45±3.83 | 11.95±2.91 | 15.75±3.33 | 0.0001* | 8.9 | 0.21 |
| p-value | 0.0001 * | 0.0001* | 0.0001 * | |||
| MD | 13.5 | 14.37 | 11.25 | |||
| Variables | A versus B (MD)(CI (95%)/ p-value) |
A versus C (MD)(CI (95%)/ p-value) |
B versus C (MD)(CI (95%)/ p-value) |
|||
|---|---|---|---|---|---|---|
| Peak to peak amplitude(µv) | -0.07(-0.27 to 0.13) | 0.99** | 0.6(0.4 to 0.8) | 0.001* | 0.68 (0.47 to0.88) | 0.001 * |
| Latency (ms) | 0.26(0.04 to 0.48) | 0.06** | -0.56(-0.78 to -0.34) | 0.001 * | -0.82 (-1.04 to -0.6) | 0.001* |
| F-wave | 0.39(-0.49 to1.28) | 0.84** | -1.12 (-2 to -0.23) | 0.008* | -1.5 (-2.4 to -0.6) | 0.001* |
| PPT | -0.54 (-0.7 to -0.3) | 0.001* | 0.8 (0.6 to 1.02) | 0.001* | 1.35 (1.14 to 1.56) | 0.001 * |
| ANDI | 0.5 (-1.89 to 2.89) | 0.99* | -3.29(-5.6 to 0.89) | 0.001* | -3.79(-6.18 to -1.39) | 0.001* |
Discussion
This study was conducted to find out the impact of SNAGS versus neural mobilization on nerve root function on peak to peak amplitude, latency, F wave, pressure pain threshold, cervical neck function in patients suffering from cervical radiculopathy. Between groups analysis: there was no statistical significant difference among three groups before treatment as p>0.05 while there was statistical significant difference among three groups post treatment as p<0.05 in all measured variables with more favor to group B. within group analysis: there was statistical substantial difference between pre as well as post-treatment in all variables in groups A as well as B, while there was only statistical substantial difference in pressure pain threshold and cervical neck function in group C as p<0.05.
Concerning the refinement in Mulligan technique (SNAGS)group on peak to peak amplitude, latency and f-wave, pressure pain threshold and cervical neck function; the improvement in this group may be attributed to the ability of Mulligan technique (SNAGS) in order to return the facet joint of the spine to its normal articular mechanics 23. The superior and inferior facets collectively create the posterior margin of the intervertebral foramen, which serves as a site where the cervical nerve roots might be compressed 24.
Mulligan technique (SNAGS) mobilization could improve the nerve function by decreasing the pressure on nerve root and correcting the positional fault, this can be achieved by separating the surfaces of the facet joints or by releasing the trapped meniscoid. Another approach is to enable the trapped meniscoid to naturally return to its original location within the joint. Alternatively, stretching adhesions may also be effective 25. Combining the cervical Mulligan technique (SNAGS) on the C5/C6 intervertebral joint with right rotation has been found to produce sympathoexcitatory responses in asymptomatic individuals. This suggests that the effect achieved by the Mulligan technique SNAGS is comparable to that of manipulation, and is likely due to a centrally mediated phenomenon 26.
The Mulligan technique (SNAGS) has been proven effective through a neurophysiological mechanism that involves the production of initial hypoalgesia. This is achieved by stimulating peripheral mechanoreceptors and inhibiting nociceptors, as well as by altering the sympathetic nervous system. Additionally, the technique operates on the biomechanical concept of correcting positional faults 20.
An further mechanism that explains pain modulation is the activation of the descending pain inhibitory system in the central nervous system 27. This approach activates the movement, which in turn stimulates the proprioceptive tissues, specifically the golgi tendon organ through tendon stretching. The Mulligan approach, also known as SNAGS, realigns the joint, allowing it to move in its intended path and gently extends the contracted soft tissues, restoring their normal flexibility. This leads to alleviation of pain and enhanced functionality 28-29.
The findings of this study come in agreement with Abdallah et al (2017) who investigated the effect Mulligan technique (SNAGS) as well as low level LASER therapy on pain, function, peak to peak amplitude and latency in patients suffering from CR 30. The results reported improvement in all measured variables in Mulligan technique (SNAGS) group. In the same line, El-Sayed et al (2017) investigated the effect of mulligan technique (SNAGS) on somatosensory evoked potential (peak to peak amplitude and latency) in patients with cervical radiculopathy and revealed that Mulligan technique has been found to enhance dermatomal somatosensory evoked potential more effectively than a traditional physical therapy programme alone in the treatment of patients with chronic cervical radiculopathy 31.
Furthermore, the results of this study align with Niaz et al (2017) who compared between mulligan technique (SNAGS) and Maitland technique in patients having CR, the findings reported improvement in pain level 32. In addition, Ojoawo et al. (2021) conducted a comparison of the effects of SNAGS as well as mechanical cervical traction in the treatment of patients having cervical radiculopathy. The study assessed the severity of pain, disability, as well as ange of motion at the beginning, as well as during the third and sixth weeks of each treatment session. The findings indicated that both SNAGS as well as mechanical traction effectively decrease disability and improve range of motion. However, SNAGS demonstrate a greater reduction in pain intensity 33.
The observed enhancements in peak to peak amplitude, latency, F-wave, pressure pain threshold, as well as cervical neck function in the NM group can be attributed to NM's capacity to influence brain structures in settings characterized by neural involvement or neural mechano-sensitivity. It is believed to affect the movement of nerve cells and their connective tissue, as well as the circulation of the nerves, by changing the pressure in the neurological system. Additionally, the dispersion of intraneuraledema can potentially reduce the excitability of dorsal horn cells 34.
Furthermore, a systematic review has provided evidence for the efficacy of NM in patients suffering from CR. The review reported that NM has the ability to alleviate symptoms of edema as well as demyelination caused by nerve root compression, as well as improve microcirculation dysfunction by restoring homeostasis between the neural tissue as well as surrounding structures. In addition, the use of NM decreased intraneural edoema, enhanced the flow of fluid between cells, decreased hyperalgesia, and stimulated the immunological response. On top of that, NM approaches have been known for being both safer and more particular in their targeting than other methods 35.
This study's findings are consistent with Savva et al (2016) who examined the impact of NM as well as cervical traction on pain levels, functionality, grip strength, as well as active range of motion in individuals diagnosed with cervical radiculopathy. The findings indicated that the combination of NM as well as cervical traction resulted in enhancements in pain reduction, functionality, grip strength, as well as the range of motion of the neck's normal joints 36.
Also, Kim et al (2017) examined the impact of NM combined with manual cervical traction versus manual cervical traction alone on pain, functional impairment, muscle endurance, as well as ROM in subjects having CR. The pain intensity scale, neck disability index, ROM, as well as endurance of the deep flexor muscles were assessed at three time points: before the experiment, four weeks, and eight weeks after, in order to compare the results. The findings demonstrated enhancement in the NM group across all examined variables 37.
In addition, Khan et al (2015) examined the efficacy of neck mobilization and NM in individuals experiencing cervico-brachial pain. Pain as well as active cervical ROM were evaluated prior to and following the intervention, as well as one week thereafter. Both strategies resulted in substantial improvement in pain levels and NDI scores at the end of the treatment 38. In the same line, Ragonese, (2009) studied the effects of therapeutic exercises on individuals suffering from cervical radiculopathy and compared them to manual treatment techniques such as cervical lateral glide, neural mobilization, as well as thoracic mobilization. There was a significant decrease in pain and NDI scores in the manual treatment group compared to the therapeutic exercise group. To reduce pain, he recommended neural mobilization in addition to therapeutic exercises for patients suffering from cervical radiculopathy 39.
Moreover, Anwar et al (2015) examined the efficacy of a conservative treatment as well as neural mobilization therapy in individuals diagnosed with cervical radiculopathy. The measurements were obtained using a visual analogue scale, while the subjects' functional status was assessed using the NDI. Upon conclusion of the study, a substantial difference in the NDI score was observed, with the NM group exhibiting a favorable outcome 22.
Conclusion
Both of Mulligan and neural mobilization have a positive effect on amplitude, latency, F-wave, PPT and neck function with more superiority to neural mobilization.
Limitation
This study had some limitations concerning the long term effect of Mulligan and NM on nerve root function was not measured so future research will be needed to claim this points. kinesiophopia and sleep quality should be measured, so future research will be needed.
Conflict of interest
There were no conflicting interests.
Sources of funding
This research received no funding from the government, the private sector, or non-profit organizations.
References
Plener, Joshua DC, Csiernik, Ben DC; To, Daphne DC; da Silva-Oolup et al (14).Conservative Management of Cervical Radiculopathy: A Systematic Review. The Clinical Journal of Pain. 2023; 39(3):p 138-146.
Buser Z, Ortega B, D’Oro. Spine degenerative conditions and their treatments: national trends in the United States of America. Global Spine Journal. 2018;8:57–67.
Lam KN, Heneghan NR, Mistry J, Ojoawo AO, Peolsson A, Verhagen AP et al (10). Classification criteria for cervical radiculopathy: An international e-Delphi study. Musculoskeletal Science and Practice. 2022; Oct 61:102596.
Lyer S Kim HJ. Cervical radiculopathy. Curr Rev Musculoskelet Med. 2016;Sep;9(3):272-80
Kim H, Nemani V, Piyaskulkaew C and Vargas S. Cervical radiculopathy: incidence and treatment of 1,420 consecutive cases. Asian Spine Journal. 2016;(10):231–237
Miranda L, Facchini D and Manfio E. Influence of cervical spine manipulation on neck joint position sense error in patients with chronic neck pain. Journal of Manual Therapeutic Posturology Rehabilitation. 2016; (14):405-413
Sari H, Akarirmak U and Uldag M. Active myofascial trigger points might be more frequent in patients with cervical radiculopathy. European journal of physical and rehabilitation medicine. 2012; 48(22):237-244.
Boyles R, Toy P, Mellon J Jr, Hayes M, Hammer B. Effectiveness of manual physical therapy in the treatment of cervical radiculopathy: a systematic review. Journal of manipulative and physiological therapeutics. 2011; Aug;19(3):135-42
Oznur B, Buket B, SenemS, Caner K and Ismail C. Clinical Study The Effect of Mulligan Mobilization Technique in Older Adults with Neck Pain: A Randomized Controlled, Double-Blind Study. Pain Research and Management. 2018;15. 2856375.
Kisner C and Colby L. Therapeutic exercise: foundations and techniques. FA Davis, philadilphia,2012;ch. 16, pp: 485-539.
Santos FM, Grecco LH, Pereira MG, Oliveira ME, Rocha PA, Silva JT et al (1). The neural mobilization technique modulates the expression of endogenous opioids in the periaqueductal gray and improves muscle strength and mobility in rats with neuropathic pain. Behavior and Brain Function. 2014; 13(10) 19.
Neto T, Freitas SR, Marques M, Gomes L, Andrade R, Oliveira R. Effects of lower body quadrant neural mobilization in healthy and low back pain populations: a systematic review and meta-analysis. Musculoskeletal Science and Practice. 2017; 27, 14e22.
Srinivasulu M and Chunduri. Comparing Mulligan Mobilization and Neural Mobilization Effects in Patients with Cervical Radiculopathy.RJPT journal of physiotherapy. 2021;1(2):31-38
Dumitru D. Somatosensory evoked potential: Electro diagnostic medicine. Belfus, H-Inc, 1st Ed. Philadelphia.1995.
Diab A and Mostafa I (2012): The efficacy of forward head correction on nerve root function and pain in cervical spondylotic radiculopathy: a randomized trial, journal of Clinical Rehabilitation. 2012; 26 (4): 351-361.
Vanderweeen L, Oostendorp RA, Vaes P and Duquet W. Pressure algometry in manual therapy. Manual Thererapy.1996; 1(5): 258–265.
Shaheen AM, Omar MT, Vernon H. Cross-cultural Adaptation, Reliability, and Validity of the Arabic Version of Neck Disability Index in Patients with Neck Pain. Pain. 2013; 38(10): 609-615.
Mac Dermid J, Walton D, Avery S, Blanchard A, Etruw E. Measurement properties of the neck disability index: a systematic review. Journal of Orthopedic and Sports Physical Therapy. 2009; 39(5):400-417.
Hing W, Hall T and Mulligan B. The Mulligan concept of manual therapy - 2nd edition.phyladilphia, 2019; Pp: 125-129.
Mulligan B. part one, spinal mobilization chapter, manual therapy, NAGS” “SNAGS” “MWMS”, 5th ed,Plane View Press, Wellington. 2004; 9-11.
Ellis RF and Hing W. Neural mobilization: A Systematic review of randomized controlled trials with an analysis of therapeutic efficiency. Journal of manipulative and physiological therapeutics.2008;16(1): 8-22.
Anwar S, Malik AN, Amjad I. Effectiveness of neuromobilization in patients with cervical radiculopathy. Rawal Medical Journal. 2015; 40: 34-6.
Exelby L. Mobilizations with movement: A personal view. Physiotherapy.1995; 81: 724-9.
Kim HS, Lee JH, Cheh G and Lee SH. Cervical radiculopathy caused by vertebral artery loop formation: A case report and review of the literature. Journal of Korean Neurosurgical Society.2010; 48: 465-8.
Hearn A and Rivett D. Cervical SNAGs: A biomechanical analysis. Manual Therapy.2002; 7: 71-9.
Moulson A and Watson T. A preliminary investi-gation into the relationship between cervical snags and sympathetic nervous system activity in the upper limbs of an asymptomatic population. Manual Therapy. 2006; 11: 214- 24.
Pamela Teys, Leanne Bisset, Natalie Collins, Brooke Coombes, Bill Vicenzio. One week time course of the effects of Mulligan’s mobilization with movement & taping in painful shoulders. Manual Therapy. 2013; 18(5):372-377.
Nicholas S Nicholas. Atlas of Osteopathic Techniques. 2nd ed. Classic Osteopathic Medical Works;1974.
Hsieh CY B,VicenzinoCH,Yang MH Hu, Yang: Mulligan’s mobilization with movement for the thumb: A single case report using magnetic resonance imaging to evaluate the positional fault hypothesis. Manual Therapy. 2002;7(1):44-49.
Abdallah GA, Mohamed RA, Sharaf MA. Effect Of snags mulligan technique versus low level laser therapy on patients with unilateral cervical radiculopathy. International journal of physiotherapy research. 2017; 5(4):2240-2248.
EL-Sayed, WH Mohamed AF, ABD EL-Monem G and. Ahmed HS. Mulligan technique provides an additional effect in treatment of chronic cervical radiculopathy patients as it improves dermatomal somatosensory evoked potential more than conventional physical therapy program alone. Medical Journal of CairoUniviersity.2017;85( 2):787-793.
Niaz M A, Zafir A, Saddique U, Bin Adel H, Akhtar S. Effectiveness of Maitland’s Mobilization vs.Mulligan Mobilization in Patients with Cervical Radiculopathy (A double blinded randomized clinical trial). Ophthalmology.2017; 15 (2):160-164.
Ojoawo AO, Nihinlola BJ, Chidozie ME, Adeyemi T. Comparative Effects of Sustained Natural Apophyseal Glides and Mechanical Traction in the Management of Cervical Radiculopathy: A Randomized Control Study. Journal of Musculoskeletal Disorder.2021;7:099.
Likhite AS, Balthillaya G, Prabhu A, Gangavelli R (2017): Effect of Upper Limb Neural Mobilization on Vibration Threshold and Hand Grip Strength in Asymptomatic Individuals: A randomized controlled trial. Journal of clinical and diagnostic Research. 2017;11(11).
Liang L, Feng M, Cui X, Zhou S, Yin X, Wang X et al (1). The effect of exercise on cervical radiculopathy: A systematic review and meta-analysis. Medici-ne. 2019; 98(45): 1-7.
Savva C, Giakas G, Efstathiou M, Karagiannis C, Mamais I. Effectiveness of neural mobilization with intermittent cervical traction in the management of cervical radiculopathy: A randomized controlled trial. International journal of Osteopathic Medicine. 2016; 21: 19-28
Kim DG, Chung SH, Jung HB. The effects of neural mobilization on cervical radiculopathy patients’ pain, disability, ROM, and deep flexor endurance. Journal of Back and Musculoskeletal Rehabilitation. 2017; 30(5): 951-59.
Khan MR, Shafi H, Amjad I, Siddiqui FA. Efficacy of Cervical Spine Mobilization Versus Peripheral Nerve Slider Techniques (Neurodynamics) in Cervicobrachial Pain Syndrome. Journal of physical therapy. 2015; 10(4): 473-79
Ragonese J. A randomized trial comparing manual physical therapy to therapeutic exercises, to a combination of therapies, for the treatment of cervical radiculopathy. Orthopedic Physical Therapy Practice. 2009; 21(3): 71-6.